Table of Contents >> Show >> Hide
Hearing the word psychosis can be scary. Movies often turn it into a horror plot twist, but in real life psychosis is a mental health symptom that real people live with, manage, and recover from every day. If you or someone you love is dealing with psychosis, you’re not dealing with a lost cause you’re dealing with a health condition that deserves calm, informed, and compassionate support.
This guide walks you through what psychosis is, how to stay safe, what treatment and recovery can look like, and practical ways to support yourself or someone else. You’ll also find real-world style examples at the end to make the advice feel more concrete and human.
Important: This article is for education only and is not a substitute for professional medical or mental health care.
What Is Psychosis, Really?
Psychosis is a condition in which a person has trouble telling what’s real from what isn’t. It’s not a diagnosis on its own it’s a symptom that can appear in conditions like schizophrenia, bipolar disorder, severe depression, or health issues like certain neurological conditions and substance use.
Common features of psychosis include:
- Hallucinations: Seeing, hearing, smelling, or feeling things others don’t (for example, hearing voices when no one is speaking).
- Delusions: Strong beliefs that don’t match shared reality (for example, being convinced you’re being targeted or followed, despite no evidence).
- Disorganized thinking and speech: Thoughts can feel jumbled; speech may jump quickly from one topic to another.
- Changes in behavior or emotions: Withdrawal, unusual behavior, or difficulty doing everyday tasks like school, work, or self-care.
Psychosis often first appears in late teens or early adulthood, but it can happen at other ages too. Early treatment especially within the first months of symptoms is strongly linked to better long-term outcomes.
When Psychosis Is an Emergency
Sometimes psychosis can become a crisis. It’s an emergency if any of the following are happening:
- The person is talking about suicide or wanting to die.
- They’re talking about harming others or seem likely to act on frightening beliefs.
- They’re so confused or disorganized that they can’t care for basic needs (eating, drinking, staying safe, shelter).
- They are acting in risky ways (wandering into traffic, handling dangerous objects, etc.).
In those situations, call your local emergency number or crisis line right away. In the United States, you can call or text 988 to reach the Suicide & Crisis Lifeline. If you do call emergency services, say clearly that this is a mental health crisis and, if possible, mention that the person is experiencing psychosis so responders can tailor their approach.
Supporting Yourself When You Experience Psychosis
Step 1: Get Professional Help Early
Early help can change the entire trajectory of psychosis. Many communities have first-episode psychosis or coordinated specialty care programsteam-based services that provide medication, therapy, family education, school or work support, and peer support all in one package.
If you’re noticing signs in yourself, here are practical first steps:
- Talk to a primary care doctor, psychiatrist, or mental health clinic and describe your experiences clearly.
- Mention specific symptoms like hearing voices, feeling watched, or being extremely suspicious, rather than just saying “I’m stressed.”
- Ask about early psychosis or coordinated specialty care programs in your area.
Getting help early is not “giving up.” It’s the mental health version of seeing a doctor quickly for chest pain instead of trying to walk it off.
Step 2: Understand Medication and Therapy
For many people, treatment includes antipsychotic medication, which can reduce hallucinations, delusions, and agitation. Different medications work differently for each person, and side effects vary, so it often takes some trial and error with a professional.
But medication is only one part of the picture. Other helpful supports may include:
- Individual therapy to build coping skills and process the experience of psychosis.
- Cognitive-behavioral therapy for psychosis (CBTp), which helps you examine and respond to distressing beliefs and experiences in more helpful ways.
- Family education and support to help loved ones understand what’s happening and how to respond constructively.
- Supported employment or education to help you return to work or school with the right accommodations and support.
Ask providers to explain your options in plain language. It’s completely okay to take notes, bring a trusted person to appointments, and ask the same question more than once.
Step 3: Everyday Coping and Grounding Strategies
While professional treatment is key, there are things you can do day-to-day to support yourself:
- Use grounding tools. When voices or beliefs feel overwhelming, focus on sensory details: name five things you can see, four you can feel, three you can hear, two you can smell, and one you can taste. This can help you reconnect with the present moment.
- Limit substances. Alcohol, cannabis, and other substances can intensify psychosis for many people. Work with a professional to reduce or avoid them safely.
- Protect your sleep. Sleep deprivation can worsen symptoms. Aim for a consistent schedule, a calming pre-bed routine, and a quiet, dark sleeping space.
- Create a stress “budget.” Stress doesn’t cause psychosis by itself, but it can make symptoms worse. If you know certain situations spike your stress, plan recovery time afterwards.
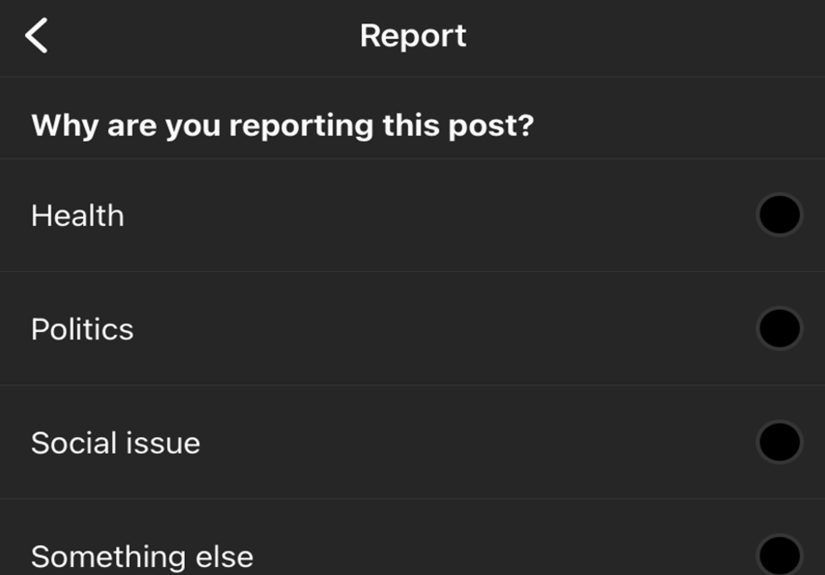
- Use technology intentionally. Constant scrolling, conspiracy videos, or stimulation late at night can be triggering. Curate your online spaces and give your brain regular breaks.
Step 4: Build Your Support Team
Psychosis can feel isolating. Building a small, trustworthy support team makes a huge difference:
- Choose one or two people you trust and tell them what you’re going through, at your own pace.
- Let them know specific ways they can help for example, “If I start getting really suspicious, please gently remind me we can call my doctor.”
- Consider a peer support group (in person or online) of people who have lived experience with psychosis. Being able to say “me too” and really mean it can be powerful.
You don’t have to share everything with everyone. It’s okay to have a “public version” and a “trusted circle” version of your story.
How to Support a Loved One with Psychosis
Start with Safety and Calm
If your loved one is experiencing psychosis, your calm presence can be incredibly grounding. Try to:
- Speak slowly and clearly, using short sentences.
- Keep your voice calm and your body language non-threatening (give them personal space; avoid sudden movements).
- Reduce sensory overload turn off the TV, lower the lights, and move to a quieter space if possible.
You don’t have to “fix” the psychosis in the moment. Your job is to help everyone stay as safe and steady as possible until more help is available.
Communicate Without Arguing About Beliefs
One of the hardest things for families is seeing a loved one hold beliefs that don’t match shared reality. It’s often tempting to argue “That’s not happening!” or “No one is following you!” but this usually backfires and damages trust.
Instead, try these approaches:
- Validate feelings, not the content. You might say, “I can see this feels really scary,” or “It sounds like you feel very unsafe,” rather than agreeing that the threat is real.
- Use “I” statements. “I’m not seeing what you’re seeing, but I can tell it’s really upsetting,” leaves room for both of your perspectives.
- Look for overlap. You may not agree on the cause, but you can agree on a goal: “We both want you to feel safer. Let’s see what could help with that.”
You’re not trying to win a debate; you’re trying to stay connected so they’re more likely to accept help and share what they’re going through.
Offer Practical, Concrete Support
Psychosis can make everyday tasks feel exhausting. Helpful supports can include:
- Offering rides to appointments or helping arrange transportation.
- Helping manage paperwork, insurance forms, or school/work communication.
- Preparing easy, nourishing meals or providing groceries.
- Helping to organize a weekly schedule with reminders for medication and appointments.
Ask, “Would it help if I…?” instead of assuming. Sometimes small, specific offers (“Can I come with you to your appointment tomorrow and take notes?”) feel easier to accept than vague offers (“Let me know if you need anything”).
Take Care of Yourself as a Caregiver
Supporting someone through psychosis can be emotionally heavy. You might feel scared, frustrated, guilty, or exhausted sometimes all in the same day. None of that makes you a bad supporter; it makes you human.
To protect your own mental health:
- Consider joining a family or caregiver support group to connect with others in similar situations.
- Schedule breaks, hobbies, and social time that have nothing to do with caregiving.
- Talk to a therapist or counselor about your stress and worries.
- Share responsibilities with other trusted friends or family members when possible.
Think of it like being on an airplane: you’re told to put on your own oxygen mask first for a reason. You can’t pour from an empty cup, and your well-being matters too.
Planning for the Future: Recovery and Relapse Prevention
Create a Crisis and Recovery Plan Together
When things are relatively calm, it’s incredibly useful to create a written plan with the person who has experienced psychosis. This plan might include:
- Early warning signs that symptoms may be returning (changes in sleep, withdrawal, increased suspiciousness, etc.).
- What has helped in the past (specific grounding strategies, trusted people to call, medications that worked).
- What hasn’t helped or feels unhelpful (for example, loud confrontations, certain phrases, or specific environments).
- Who to contact in a crisis doctors, therapists, crisis lines, trusted friends or family.
- Preferences about what should happen if they’re unable to make decisions in the moment.
This kind of plan takes some of the chaos out of a crisis and replaces it with at least a partial roadmap.
Support Lifestyle Habits that Promote Stability
While lifestyle alone cannot “cure” psychosis, healthy habits support the brain and body:
- Regular routines: Consistent meal, sleep, and activity times reduce stress on the system.
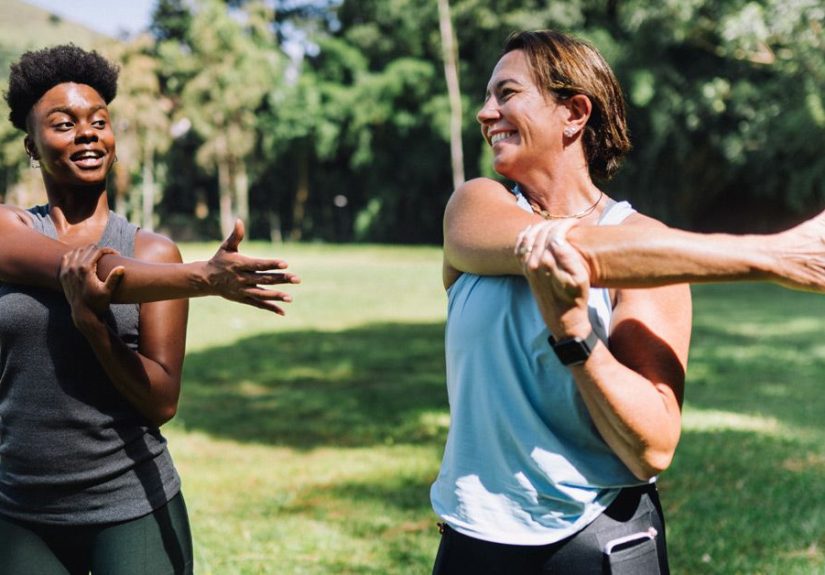
- Movement: Gentle exercise like walking, stretching, or yoga can boost mood and lower anxiety.
- Meaningful roles: Volunteering, hobbies, school, or work (with support) can rebuild a sense of purpose.
- Social touchpoints: Even a weekly coffee with a trusted person or a low-key game night can keep isolation from taking over.
Recovery from psychosis is rarely a straight line. There may be setbacks, changes in treatment, and new challenges. But many people do build lives they value with relationships, goals, and ordinary joys while also managing a vulnerability to psychosis.
Experiences: What Supporting Yourself and Others Can Look Like
To make this less abstract, imagine a few different snapshots of life with psychosis and support.
Example 1: The College Student and the First Episode
Jamie is a 20-year-old college student who starts to believe classmates are secretly recording them in class and posting the videos online. They barely sleep, stop going to lectures, and begin pacing the dorm at night, whispering to themselves. A roommate notices that Jamie seems scared and withdrawn, and instead of saying, “You’re being paranoid,” they try, “You seem really stressed and like you don’t feel safe. Do you want to talk about it?”
Jamie eventually shares that they feel watched and judged, and that it feels terrifying. The roommate doesn’t argue about whether it’s happening. They say, “I’m not seeing what you’re seeing, but I believe you’re scared. Can we go together to talk to someone at student health?” With support from campus services and family, Jamie connects to a first-episode psychosis program. They start medication, learn skills in therapy to question the most frightening beliefs, and gradually rejoin classes with accommodations.
From the outside, it might look like a sudden crisis came out of nowhere. On the inside, what helped the most was that someone noticed, stayed calm, didn’t mock their fears, and walked with them to get help instead of pushing them away.
Example 2: The Parent Who Becomes a Caregiver
Alex’s adult son, Miguel, begins experiencing psychosis in his mid-20s. At first, Alex responds the way many of us would: arguing about facts, getting frustrated, and saying things like, “You know that’s not true,” or “You’re smart, just snap out of it.” The more Alex argues, the more Miguel pulls away. Both feel misunderstood and exhausted.
After attending a family education group, Alex tries a new approach. Instead of debating whether the neighbors are spying, Alex says, “I can’t see the same thing you’re seeing, but I can tell it’s really upsetting you. I care about you, and I want you to feel safer. Can we talk about what might help you feel a little less scared tonight?” They work together on a plan: closing certain curtains, listening to calming music, and planning to call Miguel’s therapist in the morning.
Alex also starts setting boundaries and caring for their own health scheduling their own therapy, asking a sibling to help with rides to appointments, and giving themselves permission to have an occasional day off. Miguel still has hard days, but the overall relationship becomes less of a tug-of-war and more of a team effort.
Example 3: Living with Ongoing Symptoms
Not everyone’s goal is to eliminate every symptom. Sam has been living with psychosis for several years. Even with medication, they occasionally hear voices, especially when stressed. Instead of focusing only on making the voices disappear, Sam and their therapist work on changing how Sam responds to them.
They develop grounding routines: when the voices get louder, Sam texts a friend, puts on a favorite podcast, or goes for a short walk. They’ve learned to say, “I’m noticing the voices are louder today” instead of “I’m failing at recovery.” They keep a symptom journal where they track patterns: less sleep and more isolation often mean the voices get stronger, so they know to prioritize rest and connection when they see those early signs.
Friends and family support this approach by avoiding minimizing comments like, “Just ignore it” or “It’s all in your head.” Instead, they ask, “What’s helped in the past when things feel like this?” and respect Sam’s self-knowledge. Sam’s life isn’t defined solely by psychosis; they also have a job they like, a hobby they love, and a group of people who understand that “better” doesn’t always mean “symptom-free.”
Example 4: You, Reading This
Finally, there’s you the person reading this article. Maybe you’re dealing with psychosis yourself and wondering if there’s hope. Maybe you’re a friend, partner, sibling, or parent trying to figure out what to do next. Wherever you are, the fact that you’re looking for information is already a step toward understanding and support.
You don’t have to know all the answers or say all the perfect things. You don’t have to be endlessly patient or never feel overwhelmed. What matters most is continuing to move toward connection, safety, and help: making that appointment, learning about early psychosis programs, joining a support group, or simply saying, “I’m here with you; let’s figure this out together.”
Conclusion
Psychosis is serious, but it’s not a moral failing or a personal weakness. It’s a health condition that can be treated and managed, especially when help comes early and includes both professional care and human support. Whether you’re supporting yourself, a friend, or a family member, you don’t need to be perfect you just need to be present, informed, and willing to keep showing up.
Reach out for help, build a team, create a plan, and remember: recovery is often possible, progress is rarely linear, and small, steady steps forward absolutely count.