Table of Contents >> Show >> Hide
- Quick Jump (Because Your Knees Don’t Want to Scroll)
- What “Stages” of Osteoarthritis Really Mean
- Stage 1 (Minor): Early Wear & Tear
- Stage 2 (Mild): Noticeable Pain & Stiffness
- Stage 3 (Moderate): Frequent Symptoms & Limits
- Stage 4 (Severe): “Bone-on-Bone” Territory
- How Doctors Diagnose and Stage Osteoarthritis
- Treatment Options: What Works at Every Stage
- When to Seek Care ASAP (Red Flags)
- Real-World Experiences Across the 4 Stages (Extra Section)
- Conclusion
Osteoarthritis (OA) is the world’s most common “my joints are being dramatic” conditionand yes, that’s a real medical vibe.
OA happens when joint cartilage (the smooth, slippery stuff that helps bones glide) gradually breaks down. Your body, trying to be helpful,
may add extra bone (bone spurs), stiffen tissues, and stir up low-level inflammation. The result: pain, stiffness, and a joint that starts
negotiating every stair like it’s a hostage situation.
The good news: while OA can’t be “cured,” it can be managedoften very effectivelyespecially when you match the treatment plan
to the stage of the disease and your day-to-day goals.
What “Stages” of Osteoarthritis Really Mean
OA staging is a way to describe how much joint damage is present and how it tends to show up in symptoms and function.
Most “4-stage” explanations you’ll see are based on a mix of:
- Symptoms (pain, stiffness, swelling, “crunchy” sounds, reduced function)
- Physical exam (tenderness, reduced range of motion, bony enlargement)
- Imaging (usually X-ray findings like joint space narrowing and bone spurs)
Important reality check: X-rays and pain do not always match. Some people have impressive X-ray changes with mild symptoms,
while others feel significant pain before imaging looks dramatic. That’s why your experience matters as much as your images.
Also, OA doesn’t always progress in a straight line. Think of it less like a neat four-step escalator and more like a hiking trail:
some days are uphill, some are flat, and sometimes you step on a metaphorical LEGO (a flare).
Stage 1 (Minor): Early Wear & Tear
What’s happening inside the joint
Early cartilage changes may begin, and tiny bone spurs can start forming at joint edges. Many people have little to no symptoms here.
If OA staging is being described with a 4-stage system tied to X-ray grading, Stage 1 often corresponds to the earliest measurable changes.
Common symptoms
- Often no pain or only occasional discomfort after heavy activity
- Brief stiffness after sitting (the “I stood up like a rusty robot” moment)
- Subtle swelling after overdoing it
- Occasional clicking or popping that’s more weird than worrying
How it’s usually diagnosed
Many people in Stage 1 don’t get diagnosed because they don’t seek care yet. If they do, a clinician may rely on your history and exam,
and may order an X-ray if symptoms keep returningespecially in knees, hips, hands, or the spine.
Treatment goals in Stage 1
- Protect the joint by improving movement quality and strength
- Reduce risk factors (especially excess load on weight-bearing joints)
- Build habits that make later stages less likelyor less intense
Best treatments to start with
- Exercise: low-impact cardio (walking, cycling, swimming) plus strength work for supporting muscles
- Mobility: gentle stretching, range-of-motion routines
- Weight management (if relevant): even modest changes can reduce joint load
- Activity pacing: alternate “load” days with recovery days
- Supportive gear: proper shoes; sometimes inserts or braces if alignment is an issue
Stage 1 tip: If you only do one thing, build a consistent movement routine. Future-you will send a thank-you note.
Stage 2 (Mild): Noticeable Pain & Stiffness
What’s happening inside the joint
Cartilage thinning becomes more apparent. Bone spurs may be more visible, and the joint can start to lose its smooth glide.
There’s still enough cushioning that bones aren’t constantly grinding, but the joint is less forgiving.
Common symptoms
- Pain with activity (stairs, long walks, standing for long periods)
- Stiffness in the morning or after rest (often improves within minutes)
- Mild swelling or warmth after activity
- Reduced function: you begin avoiding certain movements
Diagnosis notes
This is a common stage for diagnosis. X-rays may show early joint space narrowing and osteophytes.
Your clinician will also consider other causes of joint pain and may recommend conservative treatment first.
Treatment goals in Stage 2
- Decrease pain so you can keep moving (motion is medicine, even if it’s a little annoying)
- Improve strength and mechanics to reduce stress on the joint
- Prevent flares by balancing activity and recovery
Common Stage 2 treatments
- Physical therapy: targeted strengthening (hips/thighs for knees; glutes/core for hips; grip and thumb support for hands)
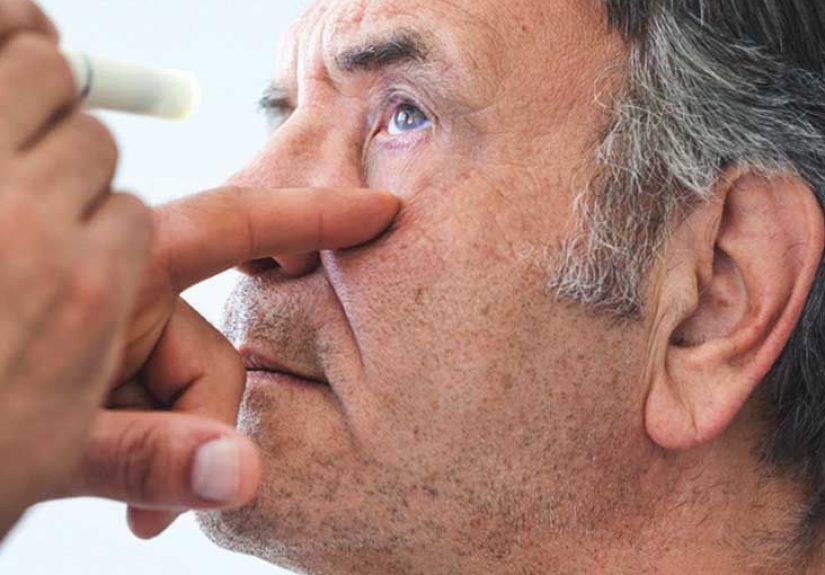
- Topical anti-inflammatory options (especially for superficial joints like knees and hands)
- Oral pain relievers/anti-inflammatories when appropriate (based on your health profile)
- Assistive supports: knee sleeves, braces, walking poles, or a cane if pain changes your gait
- Heat/cold: heat for stiffness; cold for swelling after activity
Example: A person with mild knee OA who feels pain after long walks might do a PT plan focused on quadriceps and hip strength,
adjust walking routes (flat paths first), use topical anti-inflammatory options for flares, and add cycling twice a week for low-impact conditioning.
Stage 3 (Moderate): Frequent Symptoms & Limits
What’s happening inside the joint
Cartilage loss becomes more substantial, and joint space narrowing is more pronounced. The joint may begin to change shape slightly,
and inflammation can become more persistent. This is where “I can’t ignore it anymore” often enters the chat.
Common symptoms
- More frequent pain, including during everyday activities (shopping, chores, work tasks)
- Stiffness that takes longer to loosen up
- Swelling that returns more easily
- Decreased range of motion and sometimes a visible change in joint contour
- Crepitus (grinding or crackling sensation) that may be felt more than heard
- Sleep disruption from pain in some people
Diagnosis notes
X-rays often show clearer osteophytes and definite joint space narrowing. Clinicians may discuss imaging findings alongside your functional goals:
Are you trying to keep hiking? Keep working on your feet? Open jars without inventing new swear words? (All valid.)
Treatment goals in Stage 3
- Control pain while keeping you active
- Maintain independence and function
- Reduce flare frequency and protect surrounding joints from compensation
- Consider advanced options if conservative care isn’t enough
Common Stage 3 treatments
- Structured exercise (still!) with modification: water aerobics, cycling, strength training, and balance work
- Medication strategy: topical/oral options, tailored to risks (stomach, kidney, heart, blood pressure)
- Injections: corticosteroid injections may help short-term pain and function for some joints
- Bracing/orthotics: to improve alignment and reduce load
- Assistive devices: cane, walker, jar openers, ergonomic toolsthese are “smart,” not “giving up”
- Self-management programs: education + coaching to build coping skills and consistency
Example: Someone with moderate hip OA might shift from running to cycling and strength training, use a cane during longer outings to
normalize gait, try a short course of supervised PT, and discuss an injection if pain blocks rehab progress.
Stage 4 (Severe): “Bone-on-Bone” Territory
What’s happening inside the joint
Stage 4 OA typically involves major cartilage loss. The joint space can be extremely narrowed, and bones may rub together.
Osteophytes, sclerosis (hardening), cysts, and deformity may be present. In plain language: the joint is tired, and it’s showing it.
Common symptoms
- Persistent pain, sometimes even at rest
- Major stiffness and reduced mobility
- Noticeable functional limits: walking tolerance drops; daily tasks become difficult
- Instability or “giving way” in some joints
- Reduced quality of life due to pain, sleep issues, and activity loss
Diagnosis notes
X-ray findings are usually clear in Stage 4. Your clinician may also assess alignment and nearby joints, since hips and knees love to share workloads
(sometimes unfairly).
Treatment goals in Stage 4
- Restore function as much as possible
- Reduce pain and support sleep and mood
- Decide if surgery is the best next step based on your symptoms and goals
Common Stage 4 treatments
- Comprehensive non-surgical plan: exercise modifications, assistive devices, pain management, PT for strength and safety
- Injections: may offer temporary relief for some people, though effects vary
- Surgical evaluation:
- Joint replacement (often for severe hip or knee OA when pain and disability are significant)
- Other procedures in selected cases (e.g., osteotomy or partial replacement), depending on alignment and joint compartment
Reality: Joint replacement isn’t “the easy way out.” It’s a serious, evidence-based option when OA has made your world too small.
For many people, it can dramatically improve function and painespecially when paired with rehab and strength work.
How Doctors Diagnose and Stage Osteoarthritis
OA diagnosis is usually clinicalmeaning it’s based on your symptoms, exam, and risk factorswith imaging used to confirm and stage when needed.
Here’s what that typically includes:
1) Medical history (your story matters)
- Where is the pain (knee, hip, hand, spine)?
- What triggers it (activity, stairs, gripping, weatheryes, some people notice patterns)?
- How long does stiffness last after rest?
- Any prior injuries or repetitive joint stress?
- Impact on function: walking, sleep, work, hobbies
2) Physical exam
- Tenderness, swelling, warmth (warmth can happen in OA, but marked redness and heat may raise other concerns)
- Range of motion and strength
- Crepitus (grinding sensation)
- Joint alignment and gait
3) Imaging (most often X-ray)
X-rays can show typical OA findings such as osteophytes (bone spurs), joint space narrowing (a clue for cartilage loss), subchondral sclerosis,
and cysts. Imaging also helps rule out fractures or other problems.
MRI is not always needed for straightforward OA, but it may be used when symptoms don’t match X-ray findings, when soft-tissue injury is suspected,
or when planning certain interventions.
4) Lab tests (sometimes)
OA doesn’t have a single “positive blood test.” Labs may be ordered to rule out inflammatory arthritis or other conditions if symptoms suggest them.
Joint fluid testing can be considered if gout, infection, or other causes are suspected.
A note on “staging” and grading systems
Clinicians may describe severity with a 4-stage framework (minor → severe) or use radiographic grading (often based on joint space and osteophytes).
Either way, the best staging is the one that helps guide treatment decisions and supports what you want to do with your lifenot just what an image looks like.
Treatment Options: What Works at Every Stage
OA treatment is usually a layered plan. Think of it like building a sandwich:
you want a strong foundation (movement + strength), then add smart fillings (pain control + supports), and only then consider the “toasted upgrade”
(procedures or surgery) if needed.
Non-drug treatments (the foundation)
- Exercise: strength training + aerobic activity + balance work is consistently recommended across guidelines
- Physical therapy: targeted programs for joint-specific mechanics and muscle support
- Weight management (if applicable): reduces load on hips/knees and can improve pain and function
- Education/self-management: skills for pacing, flare planning, and staying consistent
- Assistive devices: canes, walkers, braces, orthotics, ergonomic tools
- Heat/cold: heat for stiffness; cold for swelling after activity
Medications (used thoughtfully)
Medications can help, but many provide short-term symptom relief rather than long-term disease reversal. The “best” medication depends on
joint location, symptom severity, and your health risks.
- Topical options: often useful for knees and hands
- Oral NSAIDs: can improve pain and function for some people, but require risk-aware use
- Acetaminophen: may help mild pain for some; not always strong enough for moderate/severe OA
- Duloxetine: sometimes used for chronic pain patterns when appropriate
- Opioids: generally avoided when possible; reserved for specific situations under close medical supervision
Supplements note: Some supplements are popular in OA circles, but evidence is mixed and recommendations vary by product and joint.
If you want to try a supplement, do it with your clinician’s inputespecially if you take other medications.
Injections and procedures
- Corticosteroid injections: may help short-term pain and function in certain joints for some people
- Other injections: effectiveness varies; recommendations differ across guidelines and joints
- Procedural options: considered case-by-case based on symptoms, imaging, alignment, and goals
Surgery (when symptoms and function justify it)
Surgery is typically considered when pain is persistent, function is significantly limited, and a well-executed conservative plan isn’t enough.
For many people with severe hip or knee OA, joint replacement can be life-changingespecially when paired with rehab and strength work.
When to Seek Care ASAP (Red Flags)
OA is common, but not every joint problem is OA. Seek prompt medical care if you have:
- Sudden severe swelling, intense warmth/redness, or fever
- Inability to bear weight after an injury
- Rapidly worsening pain or function over days to weeks
- Severe night pain with unexplained weight loss or systemic symptoms
- A hot, swollen joint with severe tenderness (needs urgent evaluation)
Real-World Experiences Across the 4 Stages (Extra Section)
Below are common experiences people report as OA progressesshared here as realistic examples (not medical advice, and not one-size-fits-all).
The goal is to make the stages feel less like a textbook and more like something you can recognize and respond to.
Stage 1: “Is this just getting older… or did I sleep wrong?”
People often describe Stage 1 as a collection of tiny hints: a knee that feels “off” after a long day, a hip that’s stiff after a car ride,
or fingers that complain after a weekend of home projects. Because symptoms are mild and inconsistent, many people brush them off.
A common pattern is that movement helpsonce they get going, it loosens upso they assume it’s not “serious.”
The risk here isn’t immediate disaster; it’s missing the chance to build habits early. People who start strength training or PT-style exercises in Stage 1
often say they feel more in control, even if symptoms pop up occasionally.
Stage 2: “Okay, it’s showing up on my calendar now.”
In Stage 2, symptoms become predictable. Someone might notice that stairs are consistently worse than flat ground, or that a long grocery trip triggers pain later.
Many people report they begin “planning around the joint”choosing parking spots based on walking distance, avoiding certain workouts, or taking breaks during chores.
A big emotional shift can happen here: frustration. The joint still works, but it’s less cooperative. The most helpful experiences people report in Stage 2
are (1) learning what movements are safe and beneficial, (2) getting a customized exercise plan, and (3) finding pain tools that don’t derail life
(like topical options, heat/cold, pacing, and supportive footwear).
Stage 3: “I’m doing less, and I don’t like it.”
Stage 3 is often where function changes are obvious. People may describe a shrinking comfort zonefewer social outings, less travel, fewer hobbies,
or avoiding tasks that used to be automatic. They may also notice compensation: limping, shifting weight, using the “good side” more, or changing how they stand.
That compensation can trigger new pain in the back, opposite hip, or other knee. Many people report that a structured plan helps most here:
regular strength work, a walking plan that respects flare limits, and devices like braces or a cane that make movement safer and less painful.
People also commonly say that learning to treat flares earlyrather than pushing through until they crashimproves their quality of life.
Stage 4: “I want my life back.”
In Stage 4, people often report pain that feels more constant and limitingsometimes affecting sleep, mood, and independence.
The emotional experience can include grief (for lost activities), worry (about mobility), and fatigue (from ongoing pain).
Many also report a turning point: deciding they’re done negotiating with the joint every day. Some find that comprehensive non-surgical care
still helps (especially for strength, safety, and daily function), but others reach a point where surgery becomes a practical next step.
People who do well after joint replacement often describe two things: (1) they prepared with strengthening and realistic expectations,
and (2) they committed to rehab afterward. They also often say the goal wasn’t “a perfect joint”it was getting back to normal life: walking, traveling,
playing with kids or grandkids, returning to work, or simply moving without dread.
Across all stages, one theme repeats: the earlier you build a sustainable plan, the more choices you keep.
OA may be common, but feeling powerless about it doesn’t have to be.
Conclusion
The “4 stages of osteoarthritis” framework is useful because it matches real life: symptoms often start quietly, become more consistent,
then begin affecting functionand in severe cases, may require surgical solutions. But your stage is not your destiny.
The best outcomes usually come from a practical, personalized plan: consistent movement, targeted strength, smart pain control,
and timely escalation to advanced options when needed. If OA is changing what you can do day-to-day, it’s worth getting evaluated
not to collect labels, but to expand your options.