Table of Contents >> Show >> Hide
You’re getting blood drawn, an IV placed, or you’ve had a lot of pokes in the same spot lately and suddenly the vein looks weird, hurts, or just isn’t working. People often call this a “collapsed vein,” and it sounds dramatic enough to star in its own medical TV episode. The good news? It’s usually not as terrifying as it sounds. The bad news? It’s still a sign that your vein has been injured and needs a break, and sometimes it can signal something more serious.
This guide breaks down three practical ways to tell when your vein may have collapsed, how that’s different from a simple “blown vein” or IV leak, and when it’s time to stop Googling and call a doctor or 911. It’s based on reputable medical sources and written in normal human language (with a tiny sense of humor) so you can understand what’s going on and what to do next.
What Is a Collapsed Vein, Exactly?
A collapsed vein usually means the vein has been damaged so that blood can’t flow through it properly. This often happens after repeated pokes with needles or IV catheters in the same spot, especially if the vein is small, fragile, or irritated. In medical terms, a “blown vein” is a vein that’s been injured by a needle so blood leaks into the surrounding tissue (bruising, swelling); if the vein walls cave in or scar down so it can’t carry blood, people refer to that as a collapsed vein.
Collapsed veins are most common in situations like:
- Repeated blood draws or IV placements in the same vein
- Long-term IV therapy, such as chemotherapy or antibiotics
- Intravenous (IV) drug use, especially with frequent injections and poor technique
- Underlying vein disease or fragile veins due to aging or certain medical conditions
Sometimes the damage is temporary and the vein recovers with time. Other times, especially after long-term injury, the vein can be permanently scarred and no longer usable for IVs or blood draws. Either way, your body often compensates by using nearby veins but you still want to protect the ones you’ve got.
3 Ways to Know When Your Vein Has Collapsed
You can’t diagnose yourself with 100% certainty at home that’s your healthcare provider’s job. But there are three big categories of clues that something is wrong with a vein: what you see, what you feel, and how well that vein still works.
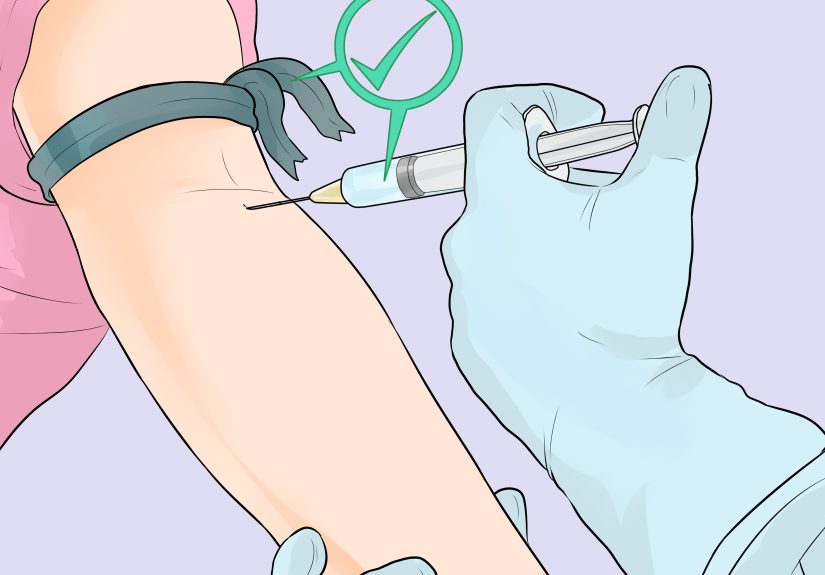
1. Look for Visible Changes Around the Vein
First, check what’s happening on the surface. A collapsed or badly injured vein often leaves some very visible “receipts” on your skin.
Common visual signs near the injection or IV site
- Bruising or discoloration: A blown or collapsed vein often leads to blood leaking under the skin. You may see a blue, purple, or even almost black patch where the needle went in.
- Swelling or puffiness: The area around the vein can look puffy or raised. This may be from blood leaking out of the vein or from IV fluid leaking into the tissue.
- Color changes beyond a simple bruise: If the skin looks unusually pale, very red, blotchy, or darker than the surrounding area, it can indicate more significant injury or circulation problems.
- Vein looks flattened or “missing”: A once-visible vein may become harder to see or feel, especially if it’s been scarred or has collapsed.
- Track marks or scarring: With long-term IV drug use or many medical sticks, you may see a pattern of tiny scars, darkened lines, or “railroad track” marks where veins have been repeatedly punctured and injured.
Mild bruising and a little swelling after a blood draw can be totally normal. What’s more concerning is when the area looks increasingly discolored, swollen, or damaged over time, or when many veins in the same area look hard, cord-like, or “burned out.”
Red flags in the way the skin looks
Call a healthcare provider right away if you notice:
- Spreading redness, warmth, and tenderness over a vein (possible inflammation or infection)
- Skin turning blue, very dark, or black near the injection site
- Open sores or ulcers around damaged veins
- Significant swelling of the whole arm or leg with color changes
These can be signs of serious vein damage, blood clots, or infection, and they’re not DIY situations they need professional care.
2. Notice How the Vein and Limb Feel
Your nerves are pretty good at screaming when something’s wrong. A collapsed or badly injured vein often comes with a specific set of sensations.
Local symptoms at the vein
- Pain or stinging at the injection site: A sharp, burning, or stinging pain during or right after a needle stick can signal that the vein has been blown or irritated.
- Ongoing tenderness: The area may stay sore to the touch, even after the needle has been removed.
- Burning or throbbing: A burning sensation along the vein or throbbing pain can indicate irritation, inflammation (phlebitis), or leakage of fluid into the surrounding tissue.
- Itching as it heals: As veins and skin heal, mild itching can appear. That can be normal healing, but intense or persistent itching with other symptoms might point to ongoing irritation or vein disease.
Changes in sensation or circulation
When a vein collapses and blood flow is impaired, you may also feel changes in the area beyond the needle stick:
- Tingling or pins-and-needles: Lack of normal blood flow or swelling around nerves can cause tingling in the hand, fingers, foot, or toes.
- Numbness or “dead arm/leg” feeling: More severe compression or circulation issues can make parts of a limb feel numb or heavy.
- Cold hands or feet: If a major vein in the arm or leg is badly damaged or clotted, the limb may feel cooler than the other side.
- Heaviness, aching, or cramping: Chronic vein problems in the legs can cause heavy, tired, or crampy sensations, especially after standing.
These symptoms don’t always mean “collapsed vein” they can also be related to blood clots, chronic venous insufficiency, or other conditions. That’s why persistent or worsening pain, swelling, or strange sensations deserve a medical check-in, not just a shrug and an ice pack.
3. Watch How Well the Vein Actually Works
The third big clue is whether the vein is still doing its job. A collapsed or badly injured vein often simply stops cooperating.
During an IV or blood draw
If you’re attached to an IV line, you and your nurse may notice:
- The IV pump keeps alarming or can’t maintain proper flow.
- The fluid is no longer dripping into the line even though the clamp is open.
- The area near the IV site starts to swell, feel cool, or look pale or tight signs the fluid is leaking into the tissue instead of flowing into the vein.
- There’s little or no blood “flashback” in the IV catheter when it’s inserted.
In simple terms: if the IV suddenly stops working and the area around it looks swollen or uncomfortable, that vein may be done for now and the line needs to be moved.
With repeated injections or long-term use
Over time, people who’ve had many injections in the same areas (whether for medical treatment or IV drug use) may notice:
- It’s getting harder to find a vein that will “take” a needle.
- Needles go in but don’t draw blood easily, or the vein collapses when suction is applied.
- Previously reliable veins feel hard, rope-like, or “dead” rather than springy.
- Staff have to move to different body areas (hands, feet, neck, groin) to find usable veins.
These are strong signs that some veins have been damaged or collapsed over time. In medical settings, this is one reason providers might recommend using a central line or port instead of constantly poking the same small peripheral veins.
Collapsed Vein vs. Blown Vein, Infiltration, and Phlebitis
People often throw around terms like “collapsed vein,” “blown vein,” and “infiltrated IV” as if they’re all exactly the same. They’re related, but not identical:
- Blown vein: A needle has punctured the vein wall so blood leaks out into surrounding tissue. You’ll see bruising, swelling, and tenderness around the site.
- Collapsed vein: The vein’s walls cave in or scar down so that blood can’t flow through it normally. This can happen after a blow, long-term irritation, or repeated needle trauma. A collapsed vein may not be usable for future IVs.
- Infiltration or extravasation: IV fluid or medication leaks out of the vein into nearby tissue, causing swelling, tightness, and sometimes pain or skin color changes. Some medications can damage tissue when this happens.
- Phlebitis / thrombophlebitis: The vein becomes inflamed, sometimes with a blood clot inside. The vein may feel like a firm, tender cord under red, warm skin.
From your point of view as the patient, all of these can mean pain, swelling, bruising, and the need for a new IV site. From your provider’s perspective, the differences matter because they determine how the vein is treated and whether there’s a risk of blood clots or serious tissue damage.
When a “Collapsed Vein” Is Actually an Emergency
Most blown or collapsed peripheral veins (for example, in your hand or elbow crease) are uncomfortable but not life-threatening. They usually heal with time, rest, and proper care. However, sometimes vein problems are part of something more serious, like a deep vein thrombosis (DVT) or pulmonary embolism (PE).
Call your doctor or seek urgent medical care right away if you notice:
- Sudden, significant swelling of an arm or leg, especially if it’s painful and warm
- Red or discolored skin along a vein with hard, tender cords under the skin
- Swelling plus visible vein distention (veins popping out more than usual)
Call emergency services (911 in the U.S.) immediately if, along with vein problems, you have:
- Sudden shortness of breath
- Sharp chest pain that worsens when you take a deep breath
- Coughing up blood
- Feeling faint, dizzy, or like your heart is racing out of nowhere
Those are classic warning signs of a blood clot that may have traveled to your lungs and that’s an emergency, not a “wait and see” situation.
What to Do If You Think a Vein Has Collapsed
Immediate steps
- Stop the injection or IV if you notice sudden pain, swelling, or discoloration around the site. If you’re in a medical setting, call your nurse or provider immediately.
- Do not keep poking the same spot. Repeated attempts in a damaged vein can make the injury worse and increase your risk of bruising, scarring, and clots.
- Elevate the limb to help reduce swelling if your provider recommends it.
- Use warm or cold compresses as directed by a healthcare provider. Some injuries respond better to warmth, others to cold don’t guess if you’re unsure.
Short-term care and follow-up
For a simple blown vein, your provider may suggest:
- Resting the area and avoiding heavy use of that limb for a day or two
- Over-the-counter pain relievers if appropriate for your health conditions
- Watching for signs of infection (increasing redness, warmth, pus, fever)
- Using other veins for future blood draws or IV placements until the area heals
If there are signs of inflammation, thrombophlebitis, or deeper vein problems, your provider might order an ultrasound, prescribe medications, or refer you to a vein specialist.
If IV or injection drug use is involved
If collapsed veins are happening because of IV drug use, it’s not just a vein issue it’s a whole-body safety issue. Repeated injections, reused needles, and contaminants can lead to severe infections, permanent vein damage, and life-threatening overdoses.
Harm-reduction and addiction-treatment programs can help with:
- Access to clean needles and safer-use education (where legally available)
- Screening and treatment for infections like HIV and hepatitis
- Support for stopping injection drug use, including medication-assisted treatment and counseling
Your veins and the rest of you will thank you for getting support, even if you’re not ready to quit immediately. The goal is to keep you alive and as healthy as possible while you figure out your next steps.
Real-World Experiences: What a “Collapsed Vein” Feels Like
Textbooks are great, but they don’t always capture what this actually feels like in real life. While everyone’s body is different, people who’ve dealt with blown or collapsed veins often describe surprisingly similar experiences. Here are some common patterns and lessons learned, pulled together from what patients frequently report.
“The IV felt fine until it really didn’t”
Many people say their IV or blood draw started out feeling normal. Then:
- They suddenly felt a sharp sting or burning that didn’t fade after a few seconds.
- The nurse or technician noticed the vein “blew” and the area started to swell.
- Discoloration (a bruise) appeared surprisingly fast sometimes within minutes.
In these cases, the vein may not truly be “collapsed” in the permanent sense, but it’s definitely injured. The body responds with leakage of blood into tissues (bruise), swelling, and tenderness. The lesson most people take away: if something feels wrong during a needle stick, speak up immediately. It’s not “being difficult” it’s protecting your veins.
“After a while, good veins are hard to find”
People who’ve had long-term treatments, like chemotherapy, dialysis, or frequent hospitalizations, often describe a gradual shift:
- At first, getting an IV was easy one stick and done.
- Over time, the same veins were used again and again.
- Eventually, those veins became scarred, less bouncy, or stopped working well for blood draws.
- Staff started hunting for new sites in hands, wrists, or even feet.
Many patients say they wish they’d known sooner that they could ask about options like using different sites, rotating veins more carefully, or discussing long-term access devices (like ports or PICC lines) if appropriate. Protecting veins early can prevent some of the “collapsed vein” problems later.
“My leg felt heavy and tight before I realized it might be a clot”
Another set of experiences comes from people who discovered that what they thought was “just a bad vein” was actually something bigger, like a blood clot. Common descriptions include:
- A calf or thigh that felt heavy, tight, or sore, especially when walking or standing
- One leg looking slightly more swollen than the other
- Skin over the vein feeling warm or looking redder than usual
- Symptoms that didn’t go away with rest, elevation, or over-the-counter pain meds
In these stories, the turning point was often a provider visit and sometimes an ultrasound confirming a clot. The big takeaway many people share afterward is: don’t ignore persistent swelling or pain in a limb, especially if you have risk factors for blood clots (recent surgery, long travel, pregnancy, certain medications, or clotting disorders). It’s easy to chalk it up to a “vein acting up,” but it can be something far more serious.
“I thought collapsed veins were just cosmetic they weren’t”
People with long-term vein issues in their legs, including collapsed or damaged veins, sometimes start with cosmetic concerns: bulging veins, color changes, or visible “spider” veins. Over time, though, symptoms often grow to include:
- Chronic aching or heaviness in the legs by the end of the day
- Swelling around the ankles or lower legs
- Darker, brownish discoloration of the skin near the ankles
- Itching, dryness, or eczema-like patches over damaged veins
- Eventually, painful sores or ulcers that heal very slowly
Many people say they waited years before seeing a vein specialist because they thought it was “just cosmetic” or part of getting older. Once they finally sought help, they often learned that early evaluation could have prevented some of the more advanced symptoms. The moral of the story: if your veins are affecting your comfort, mobility, or skin health, it’s worth getting them checked not just for how they look, but for how they function.
Big-picture takeaway from these experiences
Across all these stories, a few themes keep showing up:
- Listen to your body: Sudden pain, swelling, or weird sensations are signals to stop and investigate, not just power through.
- Speak up early: Telling your nurse or doctor something feels off can prevent worse damage to a vein.
- Protect your veins long-term: Whether you’re dealing with medical treatments or working on recovery from IV drug use, your veins are precious and worth preserving.
- Know when it’s urgent: Chest pain, shortness of breath, big limb swelling, or coughing up blood are emergency-level symptoms don’t wait those out at home.
You don’t have to become a vein expert overnight. But knowing these three main clues how the vein looks, how it feels, and how well it works can help you recognize when a vein may have collapsed, when it’s just mildly annoyed, and when it’s time to get medical help fast.







