Table of Contents >> Show >> Hide
- Quick Answer: Does MS Cause ED?
- Why MS Can Affect Erections: The “Three-Layer” Explanation
- How Common Is ED in MS?
- What ED Can Look Like in MS (And Why It Can Feel Confusing)
- Important Reality Check: MS Isn’t the Only Possible Cause
- How Doctors Evaluate ED in Someone With MS
- Treatment Options: What Actually Helps (And What Helps Most Often)
- Practical Intimacy Tips for MS-Related ED (No Weird Tricks, Just Realistic Strategies)
- When to Talk to a Clinician (Hint: Sooner Than You Think)
- FAQs: Common Questions People Don’t Always Ask Out Loud
- 500+ Words of Experiences: What Living With MS-Related ED Can Feel Like (Composite Stories)
- Experience 1: “It wasn’t just EDit was the fatigue and pressure combo”
- Experience 2: “We had to talk about it… and that was the hardest part”
- Experience 3: “Treating depression helped more than I expected”
- Experience 4: “Medication made a difference, but the ‘setup’ mattered too”
- Experience 5: “Redefining intimacy saved our relationship”
- Conclusion
Multiple sclerosis (MS) is famous for messing with nerves, balance, and energy. Less famous (but extremely real): it can also mess with sex.
If you’ve been wondering whether MS can cause erectile dysfunction (ED), you’re not imagining thingsand you’re not alone.
The short version is: yes, MS can contribute to ED, but it’s often a “team effort” involving nerves, symptoms, medications,
stress, mood, and relationship dynamics.
In this guide, we’ll break down how MS and erections are connected, what else might be going on, how clinicians usually evaluate the problem,
and what treatment options (medical and non-medical) can actually help. We’ll keep it science-based, practical, and just humorous enough to
make an awkward topic feel a little less awkward.
Quick Answer: Does MS Cause ED?
MS can cause or worsen ED because it can damage the nerve pathways in the brain and spinal cord that help coordinate arousal and sexual response.
But ED in MS is rarely caused by only one thing. Many people experience a blend of:
- Direct nerve changes from MS (the “wiring” issue)
- MS symptoms that interfere indirectly (fatigue, pain, spasticity, bladder problems, sensory changes)
- Emotional and relationship factors (stress, anxiety, depression, confidence, communication)
- General health factors that affect erections in anyone (blood pressure, diabetes, smoking, sleep, hormones)
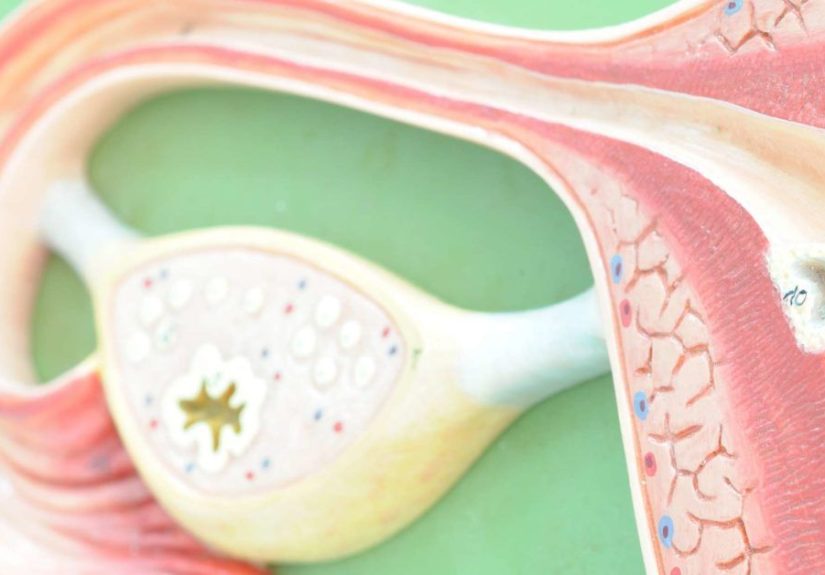
Why MS Can Affect Erections: The “Three-Layer” Explanation
Many MS specialists describe sexual dysfunction in three overlapping layers. Thinking in layers helps because it turns a scary, vague problem
into a solvable checklist.
1) Primary sexual effects (direct nerve pathway changes)
Erections involve a coordinated conversation between your brain, spinal cord, nerves, blood vessels, and hormones.
MS can interrupt the signal anywhere along that route. If the “message” doesn’t arrive clearly, the body may not respond the way you want.
Examples of primary effects include reduced genital sensation, difficulty achieving or maintaining an erection, and trouble reaching orgasm.
These can happen even when desire and attraction are still very much presentbecause desire isn’t the same thing as nerve signaling.
2) Secondary sexual effects (indirect impact from MS symptoms or treatments)
Even if the nerve pathways are mostly intact, MS symptoms can sabotage the moment. Common culprits include:
- Fatigue: the ultimate mood killer (and energy killer)
- Spasticity or muscle stiffness: when your muscles didn’t get the memo that this is not gym class
- Pain or neuropathic discomfort: hard to relax when your body is running an alert system
- Bladder or bowel symptoms: worry about accidents can block arousal
- Medication side effects: some meds for mood, blood pressure, pain, or spasticity may contribute to sexual problems
3) Tertiary sexual effects (psychological and social factors)
MS can change how people feel about their bodies, independence, and identity. That can show up as performance anxiety, lowered confidence,
depression, or stress. Relationship dynamics can shift too: sometimes a partner becomes more of a caregiver, which can complicate intimacy.
Importantly, tertiary factors are not “all in your head.” They are real, common, and treatableoften with counseling, education, and better communication.
How Common Is ED in MS?
Sexual dysfunction is widely reported in MS, and ED is one of the most common sexual concerns for men with MS.
Studies often report that sexual dysfunction affects a substantial portion of men with MS, with ED frequently mentioned as a leading issue.
The exact numbers vary because studies use different definitions, different populations, and different ways of asking sensitive questions.
Translation: it’s common enough that clinicians consider it a standard MS symptom worth discussingyet many people still feel like they’re the only one.
What ED Can Look Like in MS (And Why It Can Feel Confusing)
ED doesn’t always mean “nothing works, ever.” It can show up as:
- Difficulty getting an erection
- Difficulty keeping an erection
- Needing more time or stimulation than before
- Less reliable erections during periods of fatigue, stress, or symptom flare
- Morning erections becoming less frequent
Because MS symptoms can vary day to day, ED can also be inconsistentone day things are fine, another day your body acts like it forgot your password.
Important Reality Check: MS Isn’t the Only Possible Cause
Even if you have MS, it’s still smart to check for other common causes of EDbecause treating those can improve sexual function and overall health.
Clinicians often consider:
- Cardiovascular factors: blood vessel health strongly affects erections
- Diabetes and metabolic health
- High blood pressure
- Sleep problems (including sleep apnea)
- Hormone issues (like low testosteroneone possible factor among many)
- Depression and anxiety
- Medications that can affect sexual function
- Smoking, heavy alcohol use, and low activity
ED can be an early clue that something else is going on medically, so it’s not just about sexit’s also about long-term health.
How Doctors Evaluate ED in Someone With MS
The goal isn’t to interrogate you. It’s to figure out which “layer(s)” are driving the problem so treatment can match reality.
A typical evaluation may include:
Medical history (the useful kind)
- When the ED started and whether it’s consistent or situational
- MS symptom patterns (fatigue, spasticity, sensory changes, bladder issues)
- Mood, stress levels, relationship context
- Medication review (including antidepressants, blood pressure meds, or other relevant drugs)
- General health conditions (blood pressure, diabetes risk, sleep)
Physical exam and basic labs (when appropriate)
Depending on the situation, a clinician may check blood pressure and consider labs related to metabolic or hormonal health.
Not everyone needs extensive testing, but a baseline check can help catch treatable contributors.
Specialty referrals
Many people start with their neurologist or primary care clinician, then involve a urologist if needed.
In some cases, pelvic floor therapy or counseling/sex therapy becomes part of the planespecially when fatigue, pain, anxiety, or relationship strain are in the mix.
Treatment Options: What Actually Helps (And What Helps Most Often)
Because ED in MS is often multi-factorial, the best results usually come from a combined approacha little nervous-system strategy,
a little symptom management, a little mind-body support, and (sometimes) medication support.
1) Treat the “secondary” issues that block arousal
If fatigue, pain, spasticity, or bladder symptoms are dominating the situation, addressing those can make a major difference.
Examples of practical adjustments clinicians often recommend include:
- Timing intimacy for higher-energy windows (for many people: mornings or after rest)
- Managing spasticity triggers with positioning, stretching, warmth, or symptom-specific strategies
- Planning around bladder needs (emptying beforehand, reducing bladder irritants earlier in the day)
- Reviewing medications to see if a substitute is possible when side effects are significant
This is not “making it less spontaneous.” It’s making it more likely to work. Spontaneity is great; success is also great.
2) ED medications (PDE5 inhibitors) commonly considered
Oral prescription medications called PDE5 inhibitors are widely used for ED in the general population and are often considered for ED in MS, too.
These medications support blood flow response during sexual stimulation. They are not “instant arousal” and they don’t replace desirethey help the physical mechanism respond.
Safety matters: PDE5 inhibitors are not appropriate for everyone and can interact with certain heart medications (especially nitrates).
This is why the right move is talking with a licensed clinician who can review your health history and current meds.
3) Devices and other medical options
When pills aren’t appropriate or don’t work well enough, other options may be discussed with a urologist. These can include:
- Vacuum erection devices (a mechanical option that many people find effective with practice)
- Other prescription therapies that a specialist may consider in selected cases
- Surgical options in more refractory cases (typically after trying less invasive approaches)
The key point: there are multiple routes to the same destination, and “not responding to one option” does not mean “no options exist.”
4) Counseling and sex therapy (high value, low stigma)
If stress, depression, anxiety, relationship strain, or performance pressure is part of the picture (which is common), counseling can be one of the
highest-impact tools available. It can help you:
- Reduce performance anxiety and rebuild confidence
- Improve communication so intimacy doesn’t feel like a test
- Adapt to body changes without shame or blame
- Create realistic, satisfying intimacy routines that work with MSrather than fighting it
5) Lifestyle moves that support erections (and overall MS wellness)
Lifestyle changes won’t “cure MS,” but they can improve the general conditions that support sexual function:
- Physical activity (within safe MS limits) supports cardiovascular health and mood
- Sleep quality improves energy, mood, and hormone regulation
- Smoking cessation supports blood vessel health
- Managing alcohol helps nerve function and sexual response
- Stress reduction lowers the “fight-or-flight” signal that blocks arousal
Practical Intimacy Tips for MS-Related ED (No Weird Tricks, Just Realistic Strategies)
Because MS can be unpredictable, flexible strategies tend to work best:
Make it a team problem, not a personal failure
If you have a partner, treat the issue like: “We’re solving this together,” not “I’m failing.”
That shift alone reduces pressurepressure is basically ED’s best friend, and not in a good way.
Redefine “success” beyond one outcome
Sexual intimacy is bigger than one body part doing one job on one schedule.
When couples expand the definition of intimacy, erections often become easiernot because you forced them,
but because the nervous system relaxes.
Use timing and pacing as a tool
Fatigue is real. Planning intimacy when energy is better is not “unromantic”it’s intelligent.
Think of it as optimizing conditions, like not choosing to host a barbecue during a thunderstorm.
When to Talk to a Clinician (Hint: Sooner Than You Think)
Consider bringing it up if:
- ED persists for weeks to months
- It’s causing stress, relationship strain, or lowered confidence
- You suspect medication side effects
- You have other symptoms like reduced exercise tolerance, chest discomfort, or major mood changes
- ED appears suddenly or alongside new neurological symptoms (which may warrant MS-related evaluation)
Many people wait because it feels awkward. Clinicians have heard it all before. You won’t shock them.
(If you do, they’re in the wrong profession.)
FAQs: Common Questions People Don’t Always Ask Out Loud
Does having ED mean my MS is getting worse?
Not necessarily. ED can fluctuate with fatigue, stress, depression, medications, sleep quality, and symptom patterns.
It can also reflect general health changes unrelated to MS. That’s why a proper evaluation is helpful.
Can MS treatments help ED?
Managing MS symptoms (fatigue, spasticity, pain, bladder issues, depression) can improve sexual function indirectly.
Some people notice improvement when overall symptom control improveseven if the nerve pathway damage remains.
Is ED “psychological” if it comes and goes?
Not automatically. MS-related nerve signaling, fatigue levels, and symptom variability can create inconsistent performance.
Psychological factors can still contribute, but inconsistency alone doesn’t prove a psychological cause.
500+ Words of Experiences: What Living With MS-Related ED Can Feel Like (Composite Stories)
The experiences below are composite examples based on common clinical themes and patient-reported patternsshared to help you feel less alone
and to offer realistic, non-judgmental ideas for coping. Everyone’s situation is unique, but the emotional beats can be surprisingly similar.
Experience 1: “It wasn’t just EDit was the fatigue and pressure combo”
One common story goes like this: someone notices erections becoming less reliable, but only on certain days. At first, they assume it’s “random.”
Then they realize the bad days match high-fatigue daysafter poor sleep, after a stressful week, or during an MS symptom flare.
The frustrating part is the mental spiral: “What if it happens again?” That anxiety adds pressure, and pressure makes erections even harder.
The breakthrough for many people is reframing the goal. Instead of trying to “force performance,” they build a plan:
intimacy during higher-energy windows, longer warm-up time, and permission to pause without treating it like a disaster.
When the nervous system stops feeling chased, the body often responds more naturally.
Experience 2: “We had to talk about it… and that was the hardest part”
Another common experience is the communication barrier. A person may avoid initiating intimacy because they’re afraid of “failing,”
while their partner quietly wonders if attraction is gone. Both sides can feel rejected even when love is strong.
In many relationships, the turning point is a simple, honest conversation:
“I’m still attracted to you. My body is being unpredictable, and I’m embarrassed.”
That one sentence can lower tension and replace guessing with teamwork.
Couples who do best often agree on a “no panic” rule: if ED shows up, they switch gears rather than stop intimacy altogether.
This reduces the sense of a pass/fail exam and restores closenesseven while they pursue medical evaluation.
Experience 3: “Treating depression helped more than I expected”
MS can come with mood changes, and depression is not rare. Some people assume ED is purely neurological, then discover mood is heavily involved.
When depression improvesthrough therapy, lifestyle changes, and appropriate medical carelibido and sexual confidence can rebound.
That doesn’t mean the ED “wasn’t real.” It means the brain is part of the sexual response system, and mood can act like a dimmer switch on arousal.
Several people describe it as feeling “more present” again: less numb emotionally, less worried about performance, and more able to enjoy intimacy.
Experience 4: “Medication made a difference, but the ‘setup’ mattered too”
Some people try ED medication expecting a movie-style instant fix and feel disappointed when it doesn’t work that way.
A more realistic experience is that medication helps the physical responsebut it still depends on conditions:
fatigue level, stress, comfort, and enough time for arousal.
People who report the best outcomes often combine medical therapy with practical changes:
better timing, symptom control, and reduced performance pressure.
In other words, medication can be a powerful tool, but it’s not a magic wand that overrides exhaustion, anxiety, and spasticity.
When those pieces are addressed, many individuals describe the result as “reliable enough to relax,” whichironicallymakes reliability even better.
Experience 5: “Redefining intimacy saved our relationship”
A final, deeply human pattern: couples who thrive often expand intimacy beyond a single script.
They get creative with pacing, communication, and affection. They prioritize closeness and pleasure rather than chasing a specific outcome.
Many describe feeling like they “found their way back” to each othersometimes with help from a clinician or therapist who normalized the process.
The biggest emotional shift is this: ED stops being a secret enemy and becomes a shared challenge with a toolkit.
That’s when shame fades, pressure drops, and intimacy becomes possible againoften in ways that feel more connected than before.
Conclusion
Sodoes MS cause ED? It can, yes. MS may disrupt nerve pathways involved in sexual response, and it can also create symptoms and stressors
that make erections harder to achieve or maintain. The good news is that ED in MS is often treatable, especially when you approach it
as a multi-layer issue: nerve pathways, symptom management, general health, and emotional/relationship support.
If you take one thing from this article, let it be this: ED is not a personal failure, and it’s not a “deal with it forever” sentence.
It’s a health topicone that deserves the same problem-solving energy as any other MS symptom.