Table of Contents >> Show >> Hide
- What Is a “Breast Boil,” Exactly?
- Common Causes of Boils on or Under the Breast
- Risk Factors That Make Breast Boils More Likely
- What Do Breast Boils Look and Feel Like?
- Before You Assume It’s “Just a Boil”: What Else Could It Be?
- How Do You Treat a Breast Boil Safely at Home?
- When to See a Doctor (and What They Might Do)
- Special Situations: Breastfeeding, Nipples, and Deep Breast Lumps
- Prevention: How to Reduce the Chance of Getting Another Breast Boil
- Quick “Should I Worry?” Checklist
- Extra: Real-World Experiences People Commonly Report (and What They Wish They’d Known)
- “I thought it was an ingrown hair… until my bra declared war.”
- “I tried to pop it. It got angrier. Much angrier.”
- “Warm compresses felt too simple… but they actually helped.”
- “I was embarrassed to call a doctor… and then I got a fever.”
- “It kept coming backturns out it wasn’t ‘just boils.’”
- “I worried it was cancer. Getting checked was a relief.”
- Conclusion
A “boil” on the breast can be alarming for the same reason your phone alarm is alarming: it’s loud, it’s sudden,
and you immediately assume something terrible is happening. The good news is that many breast boils are simply
skin infections (often involving bacteria like Staphylococcus aureus) that can show up anywhere there’s
a hair follicle, friction, sweat, or a tiny break in the skin.
The not-so-fun news is that “breast boil” is a casual phrase people use for a few different problemssome minor,
some needing medical care. This article breaks down what breast boils usually are, what else they can mimic,
what you can safely do at home, what treatment looks like in a clinic, and when it’s time to stop Googling and
get professional help (spoiler: if you have fever, rapid worsening, or a painful lump that isn’t improving, call).
What Is a “Breast Boil,” Exactly?
A boil (also called a furuncle) is typically an infection of a hair follicle that creates a tender,
inflamed bump under the skin. As your immune system responds, the area can fill with fluid, pressure builds,
and the bump becomes more painful. Boils most often start when bacteria enter through a tiny cut, irritated pore,
or friction-damaged skin.
Boil vs. Abscess vs. Mastitis: Why the Words Matter
People often use “boil” to describe any painful bump with swelling. Clinically, you might be dealing with:
- Simple boil / small skin abscess: A localized skin infection that may improve with warm compresses and time.
- Larger skin abscess: A deeper pocket that often needs professional drainage (“incision and drainage”).
- Mastitis or breast infection (inside breast tissue): More common with breastfeeding, but it can occur without it. Untreated mastitis can sometimes progress to a breast abscess.
- Hidradenitis suppurativa (HS): A chronic inflammatory condition that can cause recurring boil-like lumps in skin-fold areas, including under the breasts.
Common Causes of Boils on or Under the Breast
1) Staph bacteria (including MRSA)
Many boils are caused by Staphylococcus aureus, a bacterium that can live on skin or in the nose without causing problemsuntil it finds a way into a hair follicle or small break in the skin.
Some staph infections are caused by MRSA, a strain resistant to certain antibiotics. MRSA can start as a tender bump and progress into a deeper, painful abscess. If there’s fever, rapid worsening, or it’s not improving, it’s worth getting evaluated quickly.
2) Friction + sweat + skin folds
Under-breast skin is a perfect storm: warmth, moisture, friction, and sometimes tight bras or sportswear. That environment can irritate follicles and make infections more likelyespecially during hot weather or workouts (when your underwire becomes your personal nemesis).
3) Shaving, waxing, or ingrown hairs
Any hair-removal method can irritate follicles and create small openings for bacteria. The result may look like a “pimple,” then evolve into something more painful and swollen.
4) Plugged ducts, mastitis, and breastfeeding-related infections
If you’re lactating, breast inflammation can develop quickly and may cause tenderness, redness, warmth, and flu-like symptoms. In some cases, infection can lead to a breast abscess that requires drainage.
5) Hidradenitis suppurativa (HS)
HS can cause painful, recurring lumps that resemble boils and commonly appears in areas where skin rubs togetherlike under the breasts. If you get repeated “boils” in multiple fold areas (underarms, groin, under breasts), HS is worth asking a dermatologist about.
Risk Factors That Make Breast Boils More Likely
- Close skin-to-skin friction (skin folds, heat, sweating)
- Diabetes or immune system issues (increases risk of skin infections)
- Past history of boils/abscesses or household MRSA exposure
- Smoking is linked with certain non-lactational breast inflammatory conditions (like periductal mastitis) and recurrence risk in some patterns of breast infection.
What Do Breast Boils Look and Feel Like?
Most people notice a tender bump that may feel warm, swollen, and increasingly sore over a few days. Sometimes it stays small and settles down. Other times, it enlarges and becomes more painful. It may look like a pimple at first, then behave like it has a grudge.
Symptoms that suggest a more serious infection
- Fever or feeling ill
- Rapid spreading redness or worsening swelling
- Severe pain out of proportion to the visible bump
- No improvement within 48 hours (especially if MRSA is a concern)
- A deep breast lump with redness/warmth (may suggest mastitis/abscess)
Before You Assume It’s “Just a Boil”: What Else Could It Be?
Mastitis (with or without breastfeeding)
Mastitis can cause redness, warmth, pain, swelling, and flu-like symptoms. While commonly tied to breastfeeding, it can also occur outside of lactation. If mastitis doesn’t improve or is untreated, it can lead to an abscess that may need drainage.
Hidradenitis suppurativa
HS can resemble repeated boils, often in folds and friction areas. Clues include recurring lumps, multiple sites, and episodes that come and go. Dermatology care can make a big difference.
Inflamed cysts or blocked glands
Some lumps are benign cysts or blocked skin glands that become irritated or infected secondarily.
When to rule out breast cancer
Most boils are not cancer. Still, any new breast change that doesn’t resolveespecially a persistent lump, skin dimpling, nipple changes, or unexplained dischargedeserves a clinician’s evaluation. When in doubt, get checked. (The goal is reassurance or early detection, not anxiety.)
How Do You Treat a Breast Boil Safely at Home?
If it’s small, localized, and you’re otherwise feeling okay, supportive care can help. The key word is safely.
Use warm, moist compresses
Warm compresses can encourage natural drainage and comfort. Apply a warm (not hot) compress several times a day.
This is recommended by multiple medical references for boils/abscesses.
Do NOT squeeze, pop, or “DIY lance” it
It’s temptinghumans love “quick fixes,” and pimples trained us badly. But squeezing can push infection deeper,
worsen inflammation, spread bacteria, and increase the risk of complications. Authoritative sources specifically advise
against popping or squeezing.
Keep it clean and covered
Wash gently with soap and water, avoid harsh scrubs, and cover the area with a clean, dry bandage if it’s draining.
Good hand hygiene helps protect you and everyone you live with.
Supportive comfort steps
- Wear a breathable, non-rubbing bra or soft bralette (friction is not your friend right now).
- Avoid shaving/waxing over the area until it heals.
- Over-the-counter pain relievers may help if you can take them safely (ask a clinician if pregnant/breastfeeding or if you have medical conditions).
When to See a Doctor (and What They Might Do)
It’s time to get medical care if the boil is large, extremely painful, rapidly worsening, accompanied by fever,
located near the nipple/areola with deep tenderness, or not improving within a few days of supportive care. MRSA guidance also recommends contacting a provider if there’s fever or no improvement within about 48 hours.
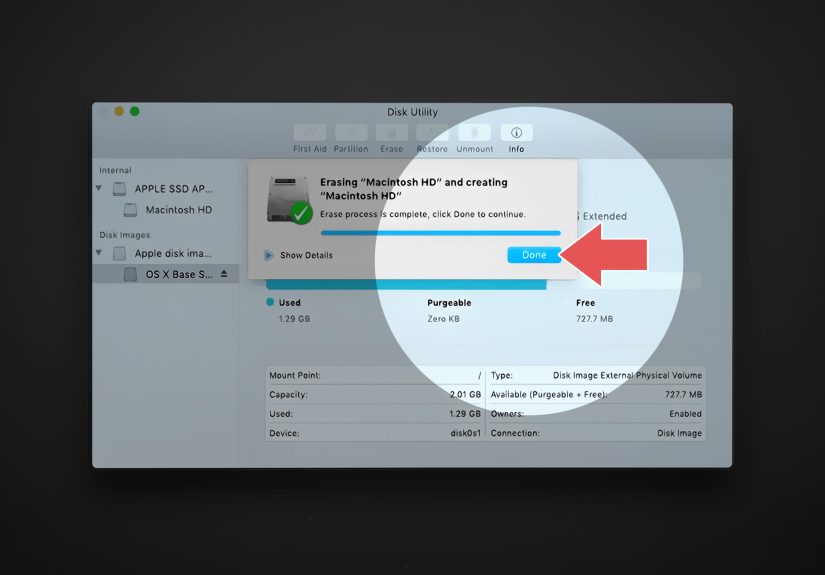
1) Confirm what it is
A clinician may examine the area and, if needed, use imaging (like ultrasound) to tell whether the problem is
a superficial skin abscess versus a deeper breast abscess. This is especially relevant in lactation-related infections
or nonlactational breast inflammation.
2) Drainage (often the main treatment for abscesses)
For many abscesses, drainage is the key step. Depending on location and depth, a clinician may drain it with a small incision or needle technique. This is not a “home project.”
3) Antibiotics (sometimes, not always)
Whether antibiotics are needed depends on the situationsize, severity, surrounding infection, fever, immune status,
and local resistance patterns. Some evidence summaries note that adding antibiotics like TMP-SMX or clindamycin to
drainage can reduce treatment failure and recurrence for uncomplicated skin abscesses, but the decision is individualized.
For breastfeeding-related mastitis, expert discussions emphasize that not every case automatically needs antibiotics
and that management depends on severity and durationanother reason it helps to get a tailored plan instead of guessing.
4) If it’s recurrent: look for the “why”
Recurrent boils can be a sign of ongoing friction/moisture issues, untreated HS, household MRSA spread, uncontrolled diabetes,
or smoking-related breast duct inflammation in certain nonlactational patterns. A clinician may discuss prevention strategies,
skin care routines, or referrals (dermatology, breast specialist) depending on the pattern.
Special Situations: Breastfeeding, Nipples, and Deep Breast Lumps
If you’re breastfeeding
If you have breast pain, redness, and flu-like symptoms, mastitis is a possibility. If symptoms don’t improve promptly,
evaluation matters because complications can include a breast abscess that requires drainage. Support resources (including
WIC breastfeeding guidance) advise contacting a clinician if you don’t feel better within about 24 hours of initial relief steps.
If the lump feels deep (not just skin-level)
A deep, firm, tender lump with redness and warmth could be mastitis or a breast abscess rather than a surface boil.
That’s a “call your provider” scenarioespecially if you feel ill or have fever.
Prevention: How to Reduce the Chance of Getting Another Breast Boil
Reduce friction and moisture
- Choose breathable fabrics; change out of sweaty clothing quickly.
- Use soft, well-fitting bras that don’t rub (underwire shouldn’t be doing woodworking).
- Keep under-breast folds clean and drygentle cleansing, pat dry.
Protect your skin barrier
- Avoid shaving over irritated skin; use clean razors and gentle techniques.
- Treat chafing early (friction can create openings for bacteria).
Limit spread (especially if MRSA is a concern)
- Don’t share towels or razors.
- Cover draining areas and wash hands often.
- Clean frequently touched surfaces if multiple household members get boils.
If boils are recurring: consider HS or metabolic factors
If you’re getting repeated boil-like lumps under the breasts or in other skin-fold areas, consider an evaluation for hidradenitis suppurativa.
And if you have diabetes or suspect blood sugar issues, getting that under control can reduce infection risk.
Quick “Should I Worry?” Checklist
- Likely okay to monitor briefly: small, superficial bump; mild pain; no fever; not rapidly worsening; improving with warm compresses.
- Call a clinician soon: not improving within 48 hours to a few days, growing, very painful, or you’ve had recurrent boils.
- Urgent evaluation: fever, rapidly spreading redness, severe symptoms, or a deep breast lump with systemic illness.
Extra: Real-World Experiences People Commonly Report (and What They Wish They’d Known)
If you’ve ever had a breast boil, you already know it’s not just “a pimple with ambition.” It can be painful, inconvenient,
and emotionally stressfulespecially because anything unusual involving breasts tends to set off the mental sirens.
Here are a few common experiences people describe, plus practical takeaways that line up with medical guidance.
“I thought it was an ingrown hair… until my bra declared war.”
A lot of people first notice a tender spot where a bra seam sits, underwire rubs, or skin folds stay damp. At first it feels
like a tiny bump. Then the friction continues, sweat joins the party, and suddenly it’s sore enough to make you walk around
like you’re carefully transporting a full cup of coffee.
Takeaway: Friction and moisture matter. Switching to a softer, breathable bra (or going braless at home if you can)
and keeping the area clean and dry can reduce irritation while it heals.
“I tried to pop it. It got angrier. Much angrier.”
This is one of the most common regret stories. Boils aren’t like typical pimples. When you squeeze, you can push infection deeper,
inflame surrounding tissue, and potentially spread bacteria. People often describe immediate worsening pain, more swelling,
or redness that expands afterward.
Takeaway: Warm compresses are the safer first move; “DIY drainage” is the fast lane to a worse situation.
Authoritative health sources explicitly recommend not squeezing or popping boils/abscesses.
“Warm compresses felt too simple… but they actually helped.”
There’s a special kind of frustration when the recommended solution sounds like something your grandma would say.
(“Have you tried… warmth?”) But moist heat can improve comfort and encourage natural drainage for minor boils/abscesses,
and it shows up repeatedly in trusted medical references.
Takeaway: Simple doesn’t mean useless. If the boil is small and you feel well otherwise, compresses plus
avoiding friction can be a solid planwhile you keep an eye on changes.
“I was embarrassed to call a doctor… and then I got a fever.”
Many people delay care because the location feels personal or awkward. But clinicians see skin infections all day, every day,
and breast boils are not a “you’re the only one” situation. Fever, feeling ill, and rapid worsening are the big neon signs that
you should get evaluated. MRSA guidance also emphasizes seeking care if symptoms include fever or don’t improve within about
48 hours.
Takeaway: Your health is more important than awkwardness. If you’re feeling sick, it’s time.
“It kept coming backturns out it wasn’t ‘just boils.’”
Recurrence is a big clue. Some people discover they have hidradenitis suppurativa (HS), especially if they also get similar
lumps in the underarms or groin. Others learn the pattern is tied to friction, sweating, or skin irritation that never fully
gets addressed. And in breastfeeding, ongoing or worsening symptoms may be mastitis-related and need a specific plan.
Takeaway: If you’re on boil number three in the same zip code of your body, ask about underlying causes and
preventionnot just “another round of dealing with it.”
“I worried it was cancer. Getting checked was a relief.”
Anxiety is normal here. Breasts change over time, and infections/inflammation can create lumps and skin changes that look scary.
People often report that the most helpful step was simply getting a professional exameither to confirm it’s an infection, start
appropriate treatment, or decide if imaging is needed.
Takeaway: If a lump or change doesn’t resolve, don’t “wait it out” indefinitely. Being breast-aware and following up
on persistent changes is smart self-care.
Conclusion
Breast boils are usually skin infectionsoften related to bacteria, friction, sweat, or irritated folliclesand many improve with
safe supportive care like warm compresses and avoiding squeezing or picking. But because the breast area can also involve deeper
infections (mastitis/abscess) or chronic conditions like hidradenitis suppurativa, it’s important to watch for red flags:
fever, rapid worsening, spreading redness, severe pain, or lack of improvement. When in doubt, get checked. The goal is quick relief,
proper treatment, and peace of mindno unnecessary suffering, and definitely no bathroom “surgery.”