Table of Contents >> Show >> Hide
- First: what “progression” really means (and why it’s so hard to stop)
- The “new era” ingredient: disease-modifying therapies (and what they canand can’tdo)
- So what’s the “new approach” that could slow progression more?
- Don’t ignore the “unsexy” slowdown tools: risk reduction and brain-protective habits
- What slowing progression can look like (realistic scenarios, not wish-casting)
- The roadblocks (because reality always shows up uninvited)
- What to watch next (the progress you can feel coming)
- Bottom line: can a new approach halt Alzheimer’s?
- Experiences related to the topic : what it feels like when “slowing” becomes real
Alzheimer’s disease has a reputation for doing what it wants, when it wantslike a cat with a PhD in stubbornness.
For decades, the best we could offer was symptom management and a lot of crossed fingers. Now, the conversation is shifting.
We’re not talking about a miracle cure (yet). But we are talking about something that would’ve sounded sci-fi not long ago:
slowing progression in some people, earlier diagnosis with a blood test, and a smarter “treat-the-whole-problem” strategy instead of
betting everything on one single target.
So could a new approach actually halt Alzheimer’sor at least slow it down meaningfully? The most honest answer is:
halting is still a stretch, but slowing is already happening for certain patients, and the next wave of progress likely comes from
doing Alzheimer’s care differentlyearlier, more precisely, and with multi-pathway plans that match the biology of the person in front of us.
First: what “progression” really means (and why it’s so hard to stop)
Alzheimer’s progression isn’t a straight line. It’s more like a messy group project where multiple biological “teams” show up late,
change the slides, and delete your notes. The classic hallmarks are:
amyloid-beta plaques (protein clumps outside neurons) and tau tangles (misfolded tau protein inside neurons).
But real-world Alzheimer’s often includes more than that: inflammation, vascular problems (blood flow issues), metabolic stress, synapse loss,
and sometimes overlapping brain diseases.
Here’s the cruel trick: the brain can compensate for damage for years. By the time memory problems are obvious, the underlying pathology
may have been quietly building. That’s one reason why past trials failedmany treatments arrived at the party after the cake was gone
and the chairs were already stacked.
The “new era” ingredient: disease-modifying therapies (and what they canand can’tdo)
The biggest shift in recent years has been the arrival of disease-modifying therapiestreatments aimed at the biology of Alzheimer’s,
not just the symptoms. In the U.S., anti-amyloid monoclonal antibodies have moved from “theory” to “clinic,” with FDA-approved options
for people in early symptomatic Alzheimer’s (typically mild cognitive impairment due to Alzheimer’s or mild dementia due to Alzheimer’s).
Anti-amyloid antibodies: why they matter
These drugs are designed to help the immune system clear amyloid plaques from the brain. Clinical trials have shown that plaque reduction can
be substantial, and for some patients this correlates with a modest but meaningful slowing of cognitive and functional decline
over time. Think of it as turning down the speed of the diseasenot putting it in reverse.
That distinction is important. Slowing progression can mean more months of independence, more time recognizing loved ones, more time handling
daily tasks without constant help. It’s not flashy like a Hollywood “instant cure,” but for families living it, extra time with better function
is the most valuable currency on earth.
But there’s a catch: who the drugs are for (and how you prove it’s Alzheimer’s)
These therapies are not “any memory problem = infusion time.” They’re intended for people in the early stages whose Alzheimer’s pathology
is confirmedtraditionally via amyloid PET imaging or cerebrospinal fluid (spinal fluid) testing.
Here’s where the new approach gets exciting: in 2025, the FDA cleared the first blood test intended to help diagnose Alzheimer’s-related amyloid pathology
in symptomatic adults above a certain age threshold. That’s a big deal because it opens the door to earlier, more accessible evaluationespecially in places
where PET scans are scarce or cost-prohibitive.
Safety is part of the story (ARIA and monitoring)
Anti-amyloid antibodies come with real risks, particularly ARIA (amyloid-related imaging abnormalities), which can include brain swelling
(ARIA-E) and small bleeds or iron deposits (ARIA-H). Many cases are asymptomatic and found on MRI, but some can cause headaches, confusion,
dizziness, vision changes, or more serious complications.
That’s why monitoring matters. Treatment protocols typically include baseline MRI and follow-up MRIs at scheduled intervals, and FDA communications have emphasized
the importance of earlier MRI monitoring for certain regimens. It’s also why clinicians discuss medications like anticoagulants (blood thinners) and genetic risk
factors (such as APOE ε4 status) when weighing benefits and risks.
So what’s the “new approach” that could slow progression more?
If you boil the next chapter down into one idea, it’s this:
Alzheimer’s won’t be beaten by a single silver bulletso we’re building a toolkit.
The new approach is not only “new drug,” but a new system:
detect earlier + treat precisely + target multiple pathways + track response like we mean it.
1) Detect earlier (before the brain has to work overtime to hide damage)
Earlier detection used to mean waiting until symptoms became undeniable. Now it increasingly means combining:
cognitive screening, medical history, imaging when needed, and biomarkers (including blood-based biomarkers as they become validated and available).
The point is simple: if a therapy works best in early Alzheimer’s, you need a reliable way to find early Alzheimer’s.
Practically, this could look like: a patient reports persistent memory changes; the clinician rules out reversible causes (thyroid issues, B12 deficiency,
medication effects, sleep apnea, depression); then uses biomarker tools to determine whether Alzheimer’s pathology is likely involved.
The goal is fewer “shrug” diagnoses and more targeted decisions.
2) Treat precisely (right patient, right stage, right risk profile)
Precision in Alzheimer’s care means matching treatment to the person’s biology and real-world situation, including:
stage of disease, comorbidities (like hypertension or diabetes), MRI findings, medication list, and risk tolerance.
It also means being honest about goals: slowing decline, preserving function, supporting caregivers, and planning ahead.
Precision also means not treating when the risk outweighs the benefit. That can feel emotionally brutallike being told you can’t board a plane to hope-ville.
But it’s also a sign the field is maturing: better to choose wisely than to treat blindly.
3) Combine therapies over time (because biology is not a one-lane road)
The most promising “new approach” is the move toward combination thinking. Alzheimer’s biology involves amyloid, tau, inflammation, synaptic dysfunction,
vascular health, and metabolic stress. So the next generation of care is likely to blend:
- Amyloid-lowering therapies (when appropriate)
- Tau-focused therapies (in development and being refined after mixed trial results)
- Anti-inflammatory / immune-modulating strategies that target harmful neuroinflammation without shutting down helpful immune function
- Vascular risk management (blood pressure, diabetes, cholesterol), because brain blood flow is not optional
- Lifestyle and cognitive resilience strategies (exercise, sleep, hearing correction, social engagement)
Combination doesn’t necessarily mean “ten drugs at once.” It can mean a staged plan: reduce amyloid burden early, then add or switch to approaches
that protect synapses, reduce inflammatory damage, or target tau spreadguided by biomarkers and clinical response.
4) Track response like a modern chronic disease (measure, adjust, repeat)
Historically, Alzheimer’s care often felt like: “See you in six months; we’ll compare notes and hope.” The new approach borrows from oncology and cardiology:
measure what you can, track change, and adjust.
That includes:
functional scales (how daily life is going), cognitive testing, caregiver reports, and when appropriate, biomarker trends.
It also includes practical outcomes: fewer falls, better medication adherence, safer driving decisions, reduced caregiver burnout.
Progress isn’t just a test scoreit’s whether Tuesday is manageable.
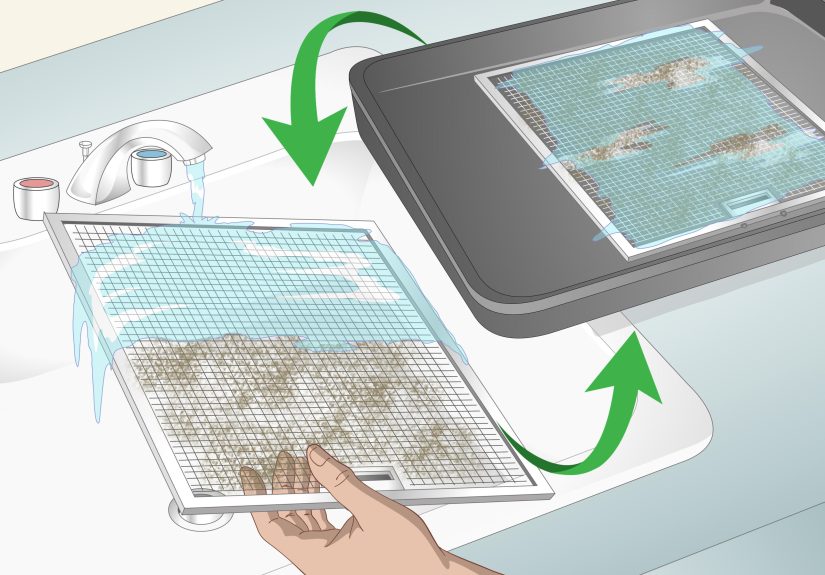
Don’t ignore the “unsexy” slowdown tools: risk reduction and brain-protective habits
Here’s the part nobody puts on a billboard because it doesn’t sell like a blockbuster drug:
vascular and lifestyle factors matter. Not because they “cure” Alzheimer’s, but because they can reduce the load on a vulnerable brain.
A brain dealing with Alzheimer’s pathology does worse when it’s also dealing with uncontrolled blood pressure, poor sleep, unmanaged diabetes, untreated hearing loss,
depression, isolation, or inactivity.
Public health guidance emphasizes actions like staying physically active, managing blood pressure, preventing or correcting hearing loss,
managing diabetes, avoiding smoking, and limiting heavy alcohol use. These steps support brain health and may reduce dementia risk or help preserve function.
Even after diagnosis, these choices can influence quality of life and resilience.
A concrete example: hearing loss and cognition
Untreated hearing loss is linked to cognitive decline and dementia risk. When hearing is impaired, the brain has to allocate extra resources to decoding sound,
leaving less bandwidth for memory and thinking. Hearing loss can also increase isolationanother hit to cognitive stimulation.
Addressing hearing (with evaluation and hearing aids when appropriate) is a surprisingly powerful “slowdown” lever.
Another example: blood pressure as brain protection
High blood pressure can damage blood vessels and reduce healthy blood flow in the brain. Managing it helps reduce stroke risk and may protect
against vascular contributions to cognitive impairmentwhich often stack on top of Alzheimer’s pathology like a bad sequel nobody asked for.
What slowing progression can look like (realistic scenarios, not wish-casting)
Let’s make this tangible. Here are three realistic, simplified examples of how a “new approach” might play out:
Scenario A: Early diagnosis + targeted therapy + tight risk-factor control
A 67-year-old notices increasing word-finding difficulty and misplacing items beyond their normal baseline. Workup rules out reversible causes.
Biomarker testing supports Alzheimer’s pathology. The patient is eligible for an anti-amyloid therapy and agrees to MRI monitoring.
At the same time, they get aggressive about blood pressure, start a tailored exercise program, treat sleep apnea, and correct hearing loss.
The combined effect: not a cure, but a better shot at preserving independence longer than “do nothing and hope.”
Scenario B: Not a candidate for infusionbut still a strong plan
A 74-year-old has cognitive symptoms but also has MRI findings and medical factors that make infusion risk too high.
Instead of a dead end, the plan emphasizes caregiver training, occupational therapy for safety, medication optimization, mood treatment,
hearing/vision correction, structured routine, and vascular risk management.
Progression may still occur, but day-to-day function can improve and crises can be delayed.
Scenario C: Research participation and combination horizons
A person with strong family history enters a research program with biomarker tracking. They join a prevention-focused lifestyle program and a clinical trial
evaluating a non-amyloid target (for example, tau or neuroinflammation pathways). This doesn’t guarantee benefit, but it reflects where the field is headed:
earlier detection, earlier intervention, and better mapping of who benefits from what.
The roadblocks (because reality always shows up uninvited)
If we’re serious about slowing Alzheimer’s progression, we have to be honest about barriers:
- Access and infrastructure: Infusion capacity, MRI availability, specialty clinics, and follow-up systems aren’t evenly distributed.
- Cost and coverage: Even with coverage pathways, out-of-pocket costs, travel, and time off work can be heavy.
- Safety and selection: ARIA risk requires careful screening and monitoring; not everyone is an appropriate candidate.
- Equity in research and care: Trials and specialty access don’t always reflect the diversity of people affected by Alzheimer’s.
- Expectation management: “Slowing” can be meaningful, but it’s not the same as “restoring.” Families deserve clarity.
What to watch next (the progress you can feel coming)
The next few years are likely to focus on:
better blood-based diagnostics, smarter risk stratification (including MRI and genetics where appropriate),
and combination trials that target amyloid plus other pathways.
There’s also intense interest in therapies that protect synapses, reduce harmful inflammation, and address tau biology more effectivelylearning from
what worked (and didn’t) in earlier generations of trials.
Another major shift is cultural: Alzheimer’s is increasingly treated like a disease with a biological timelineone where earlier detection and earlier intervention
can change outcomes. That mindset alone is a new approach.
Bottom line: can a new approach halt Alzheimer’s?
Halting Alzheimer’s completely is still a goal rather than a standard outcome. But slowing progression is no longer hypothetical.
The “new approach” isn’t a single drugit’s a strategy:
find it earlier, confirm the biology, treat the right patients, monitor carefully, combine interventions, and support the whole life around the diagnosis.
It’s not magic. It’s not instant. But it’s real progressbuilt from better science, better tools, and a willingness to treat Alzheimer’s like the complex,
multi-system problem it actually is.
Experiences related to the topic : what it feels like when “slowing” becomes real
Alzheimer’s research is often described with numberspercent slowing, points on rating scales, biomarker ratios. But the lived experience of a “new approach”
shows up in quieter places: the calendar, the kitchen, the car keys, and the emotional weather inside a family.
The following experiences are composite examples based on common patterns clinicians and caregivers reportshared here to illustrate what “slowing progression”
can mean in daily life (not as medical advice or a promise of outcome).
Experience 1: The diagnosis feels different when it comes with options.
In the past, many families recall the moment of diagnosis as a door closing: “This is Alzheimer’s. Here’s a prescription to help symptoms. See you later.”
Now, some families describe a different kind of appointmentstill painful, still heavy, but threaded with a plan.
There’s talk of staging, confirmation of amyloid pathology, whether an infusion therapy makes sense, what MRI monitoring would look like,
and how to build a support system that’s proactive instead of purely reactive.
Even when a person isn’t a candidate for an anti-amyloid drug, a structured plantreating sleep apnea, correcting hearing loss, adjusting medications that worsen cognition,
and building routinescan feel like turning the lights on in a room that used to be dark.
Experience 2: “Slowing” is not a headlineit’s a collection of Tuesdays.
Caregivers often describe progression in practical terms: fewer meals cooked, more missed appointments, trouble paying bills, repeating questions,
wandering, personality changes, and eventually needing constant supervision. When progression slows, the changes can be subtle but profound:
the person still helps fold laundry; they can follow a familiar recipe with fewer prompts; they manage a short trip to the store with a written list;
they keep their sense of humor at family dinner.
Nobody throws a parade because “Dad only got lost once this month instead of three times,” but that kind of difference changes stress levels,
safety planning, and the emotional tone of a household.
Experience 3: Monitoring becomes its own mini-journey.
The new era of treatment brings a new rhythm: infusion schedules, MRI appointments, symptom check-ins, and constant “Is this a side effect or just a bad day?”
Some people find the structure reassuring. Others find it exhaustingespecially if they live far from a specialized center.
Families talk about learning a new vocabulary (ARIA, biomarkers, staging) and navigating decisions like genetic testing.
For some, the monitoring schedule becomes a reminder that this is serious medicine, not a wellness trend. The upside is that it can also create a sense of partnership:
the clinic is watching closely, responding quickly, and making adjustments rather than waiting for a crisis.
Experience 4: Lifestyle changes feel less like “advice” and more like a prescription for dignity.
Once Alzheimer’s enters the picture, many people suddenly take “boring” habits seriously. Blood pressure control isn’t about a number on a cuffit’s about protecting
the brain’s remaining resilience. Exercise isn’t about beach seasonit’s about sleep, mood, mobility, and reducing fall risk.
Treating hearing loss becomes a way to stay socially connected, which can protect mood and reduce isolation.
Families sometimes describe a shift from “we should probably do that” to “this is part of the treatment plan,” and that mindset can improve follow-through.
Experience 5: The hope is realbut it matures.
Early on, hope can look like denial: “Maybe this will all go away.” With time, many families report a different hope:
“Let’s protect what we have, plan for what may come, and keep life meaningful.” The new approach supports that kind of hope.
It says: we can measure more, target more, monitor better, and support families earlier. It also says: we will be honest when something helps a little,
and we’ll keep pushing for the breakthroughs that help a lot.
That’s not the Hollywood ending, but it’s something far more usefulprogress you can live inside.