Table of Contents >> Show >> Hide
- Quick refresher: What earwax does (and why color changes happen)
- Why earwax can look black
- Black earwax: When it’s probably fine vs. when to get checked
- How a clinician figures out the cause
- Treatments that actually work
- 1) Do nothing (yes, that’s a legitimate plan)
- 2) Use wax-softening drops (cerumenolytics)
- 3) Gentle irrigation (only for the right situation)
- 4) Professional removal (often the fastest fix)
- 5) If infection is the cause: treat the infection (and clear the debris)
- 6) If skin irritation/eczema is contributing
- What NOT to do (your ear’s official “nope” list)
- Prevention: Keep the wax, lose the drama
- FAQ
- Bonus: Real-world experiences people commonly report (about )
- Final takeaway
- SEO tags (JSON)
Finding black earwax can feel like your body just launched a surprise Halloween update. But in many cases, dark or nearly black wax is simply
older earwax that’s had time to dry out, oxidize, and collect tiny bits of dustbasically, your ear’s version of a lint roller.
Still, “often harmless” isn’t the same as “always harmless.” Black earwax can also show up with a cerumen (earwax) impaction (a blockage),
a small amount of blood from an irritated ear canal, or an ear canal infectionincluding fungal infections that can create
dark specks or debris.
This article breaks down the most common causes, the signs that you should get checked, and the treatments that actually helpwithout turning your ear into a DIY
construction site. (Yes, that’s a polite way of saying: please don’t go spelunking with cotton swabs.)
Quick refresher: What earwax does (and why color changes happen)
Earwaxalso called cerumenisn’t “gross stuff your body forgot to delete.” It’s protective. Wax helps trap dust and debris, moisturizes the ear
canal, and can make life harder for germs. Your ears are also built to be self-cleaning: jaw movement (talking, chewing) and natural skin migration help move old
wax outward, where it flakes off or washes away during normal bathing.
Color changes are often about age and environment. Newer wax may be pale yellow or amber, while older wax tends to darken as it sits longer,
dries out, and mixes with debris. That darker shade can look brown, deep brown, orunder certain lightingalmost black.
Why earwax can look black
Think of black earwax as a clue, not a diagnosis. Most causes fall into a few buckets, and the “right” bucket depends on your symptoms, habits, and how long it’s been happening.
1) Old earwax + trapped debris (the most common, least dramatic reason)
If wax hangs around longer than usual, it can darken and dry out. Add a little everyday debris (dust, tiny fibers, outdoor grime), and you may get wax that looks
very darksometimes nearly black. This is especially common if you work in dusty environments, wear earbuds often, or use earplugs regularly.
2) Earwax impaction (a.k.a. “the wax traffic jam”)
Impaction happens when wax becomes packed into the ear canal and blocks the normal outward movement of wax. The result is often darker,
thicker waxsometimes blackbecause it’s older and compressed.
Common reasons people get impacted earwax include:
- Using cotton swabs or other objects in the ear canal (often pushes wax deeper instead of removing it)
- Narrow or curvy ear canals (your anatomy is doing its own thing)
- Frequent earbud/earplug use or hearing aids (can block wax from migrating outward)
- Dry or sticky wax that doesn’t move easily
Impaction is one of the most common reasons people feel “plugged,” notice muffled hearing, or suddenly become very aware that they have ears.
3) A small amount of blood mixing with wax
The ear canal skin is delicate. Scratching (even unintentionally) can cause a tiny amount of bleeding that mixes with earwax. As that small amount of blood dries,
it can darken wax and make it look brown-black. This can happen after using cotton swabs, fingernails, or “ear tools” that are marketed like tiny excavators
(your ear does not need archaeology).
4) Fungal or bacterial ear canal infection
Sometimes black earwax isn’t actually “wax” aloneit’s wax mixed with infectious debris. A fungal ear infection (otomycosis)
can produce dark dots or specks and may come with itching, fullness, flaking, or discharge. Certain fungi (like Aspergillus) are especially known for
dark spotting or debris in the canal.
Otitis externa (often called “swimmer’s ear”) can also cause irritation, swelling, pain, or drainage. Bacterial infections are common; fungal
infections are less common but can be stubborn and usually need targeted treatment.
5) Less common (but worth knowing) possibilities
- Foreign material: Small particles (sand, dirt, makeup, hair product residue) can mix with wax and darken it.
- Skin conditions: Eczema/dermatitis can increase flaking and irritation, which changes what comes out of the ear.
- Overuse of drying agents: Frequent peroxide-based cleaning can irritate skin and set up a cycle of dryness → itching → scratching → darker debris.
Black earwax: When it’s probably fine vs. when to get checked
Often “watch and wait” (if all of these are true)
- No pain
- No itching that’s intense or persistent
- No foul odor or unusual drainage
- No meaningful hearing change
- The wax is coming out on its own (small amounts)
Get medical evaluation soon (especially if you notice)
- Ear pain (especially worsening pain)
- Drainage that’s persistent, smelly, or not wax-like
- Hearing loss, significant muffling, or a blocked/full feeling
- Intense itching that doesn’t improve
- Dizziness/vertigo or ringing that’s new and persistent
- Visible blood or repeated blood-tinged wax
- A history of ear tubes, a perforated eardrum, or ear surgery (home irrigation may be unsafe)
If symptoms are significant, the goal is simple: confirm what you’re looking at (wax vs. infection vs. injury) and choose the safest removal or treatment method.
How a clinician figures out the cause
Diagnosis is usually straightforward: a clinician looks in your ear with an otoscope. That exam can show whether wax is impacted, whether the ear
canal skin is inflamed, and whether the eardrum appears intact. If infection is suspectedespecially fungalclinicians may remove debris and sometimes take a sample
to guide treatment.
This is why guessing based on color alone isn’t ideal. Dark wax can be harmless; it can also be wax sitting on top of a problem that needs attention.
Treatments that actually work
The best treatment depends on the cause. Here are the options that align with evidence-based ear care and professional guidelines.
1) Do nothing (yes, that’s a legitimate plan)
If you have no symptoms and wax is coming out normally in small amounts, you may not need to “treat” anything. Over-cleaning can irritate the ear canal and
increase the chance of impaction. For routine hygiene, wiping the outer ear with a damp cloth is usually enough.
2) Use wax-softening drops (cerumenolytics)
If wax seems thick, dry, or slow to come out, ear drops can soften it so it exits naturally or is easier to remove. Common options include:
- Carbamide peroxide (widely sold OTC for earwax softening)
- Mineral oil or baby oil (often helpful if your ears feel dry/itchy)
- Glycerin (a gentle softener)
Practical tip: If your ear canal gets dry and itchy easily, oil-based drops may feel gentler than frequent peroxide-based products.
Important safety note: Avoid ear drops or home wax removal if you have ear pain, drainage, a known eardrum perforation, ear tubes, or recent ear surgeryget evaluated first.
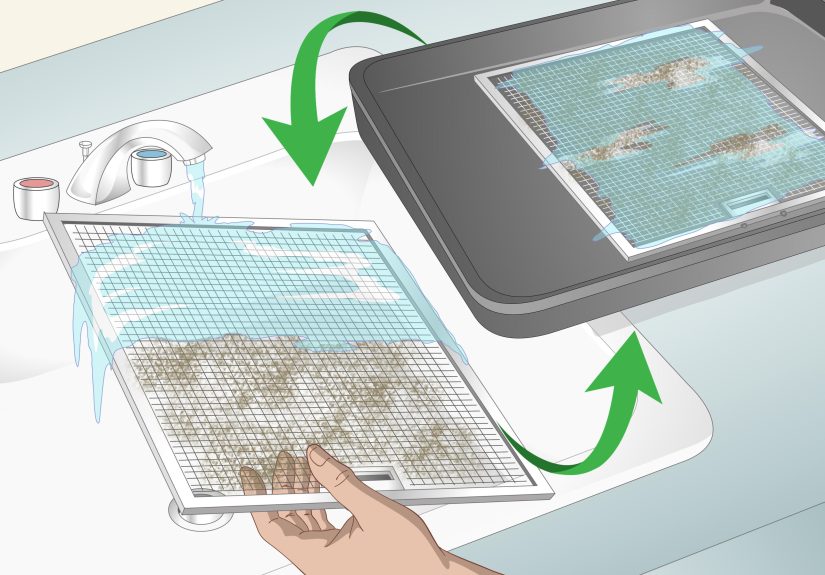
3) Gentle irrigation (only for the right situation)
Irrigation can help flush softened wax out, but it has to be done correctly. Clinicians typically use warm (body-temperature) water to reduce
discomfort and avoid dizziness. At home, irrigation kits exist, but they aren’t for everyone.
Do not irrigate if you have:
- Ear pain or active infection symptoms
- Drainage that isn’t clearly wax
- A known or suspected perforated eardrum
- Ear tubes or prior ear surgery (unless a clinician specifically okays it)
When in doubt, skip the home irrigation and choose professional removal. Your ear canal is not the place to “learn by doing.”
4) Professional removal (often the fastest fix)
In a clinic, a provider can remove wax using specialized tools (like a curette), suction, or controlled irrigation. This is especially helpful
when wax is impacted, very hard, or causing symptoms. It’s also the safest route if you’re unsure whether your eardrum is intact.
5) If infection is the cause: treat the infection (and clear the debris)
If the ear canal is infected, treatment usually starts with careful cleaning so drops can actually reach the skin. After that:
- Bacterial otitis externa is commonly treated with prescription ear drops (sometimes combined with a steroid to reduce swelling).
- Fungal otomycosis is treated by cleaning plus antifungal drops. Some cases need repeated cleaning and follow-up because fungal debris can cling and recur.
Keeping the ear dry is a big deal during treatment. Moisture can encourage ongoing irritation and make fungal problems harder to fully clear.
6) If skin irritation/eczema is contributing
If you’re stuck in a cycle of dryness → itching → scratching → darker debris, the fix may be less about “removing wax” and more about calming skin.
A clinician may recommend strategies to protect the ear canal skin, avoid irritants, and treat underlying dermatitis.
What NOT to do (your ear’s official “nope” list)
- Don’t put cotton swabs inside the ear canal. They often push wax deeper and can injure delicate skin.
- Don’t use ear candling. It doesn’t reliably remove wax and can cause burns and other injuries.
- Don’t use sharp objects (bobby pins, keys, tweezers, “ear picks”)even if the internet says you’re “built different.”
- Don’t over-clean with peroxide or frequent DIY flushes, especially if your ears are prone to dryness or irritation.
Prevention: Keep the wax, lose the drama
You can’t (and shouldn’t) eliminate earwax entirely. But you can reduce impaction and irritation with a few habits:
- Clean only the outer ear with a washcloth; let the canal handle itself.
- If you wear earbuds/earplugs/hearing aids, give your ears breaks and clean devices regularly.
- If you’re prone to buildup, ask a clinician about a maintenance plan (occasional softening drops or periodic professional cleaning).
- For swimmers: keep ears dry after swimming (tilt head, towel-dry outer ear). If you get repeated swimmer’s ear, ask about preventive strategies.
FAQ
Is black earwax normal?
It can be. Dark wax often means older wax or wax mixed with debris. “Normal” depends on symptomsif you have pain, itching, drainage, or hearing loss, it’s worth getting checked.
Can black earwax mean infection?
Sometimes. Fungal ear infections can produce dark specks or debris and are often itchy. Bacterial infections more often cause pain and swelling, but both can cause discharge.
Does black earwax mean you need to remove it?
Not always. If it’s not causing symptoms and it’s coming out on its own, you may not need treatment. Over-removing wax can irritate the canal.
What’s the safest at-home approach?
For mild wax buildup without pain or drainage, wax-softening drops can help. Avoid digging tools. If you’re unsure about your eardrum or symptoms, professional removal is safest.
How long should I wait before seeing a clinician?
If you have hearing changes, persistent fullness, pain, drainage, or intense itching, don’t “wait it out” for weeks. Those symptoms are exactly when an exam is most useful.
Bonus: Real-world experiences people commonly report (about )
The tricky thing about black earwax is that people often discover it during totally ordinary momentslike cleaning the outer ear after a shower or noticing a dark smudge on an earbud.
Here are a few common, real-life patterns clinicians hear (these are composite examples meant to reflect typical experiences, not specific individuals).
The “earbuds all day” moment
Someone who wears earbuds for work calls, podcasts, and the gym starts noticing dark wax on the silicone tips. There’s no painjust a gradual “muffled” feeling after long days.
In many cases, the earbuds act like a stopper, slowing the natural outward movement of wax. The wax sits longer, gets darker, and collects more debris. A simple fix might be
taking device breaks, cleaning earbuds often, and using occasional softening dropsunless symptoms suggest impaction that needs professional removal.
The well-intentioned cotton swab cycle
Another common story starts with “I just wanted them to feel clean.” A person uses cotton swabs regularly, but instead of removing wax, they push it deeper. Over time the wax
becomes compacted and darker. Sometimes there’s mild soreness or a small amount of blood-tinged wax after a “deeper clean,” which then dries and looks almost black.
The biggest turning point is usually learning that the ear canal doesn’t need routine scrubbingouter ear onlyplus an exam if fullness or hearing loss shows up.
The swimmer with an itchy ear
Someone who swims frequently notices itching, a full feeling, and dark specks mixed with wax. They may try drying the ear aggressively or using repeated peroxide, which can irritate
the canal further. In these cases, clinicians often think about otitis externa, including fungal causes, especially if itching is the headline symptom.
Treatment tends to work best when the canal is gently cleaned and the correct drops are usedplus a strict “keep it dry” phase during recovery.
The “my ears are just dry” experience
People with eczema, allergies, or generally sensitive skin sometimes describe flaky, irritated ear canals. They may notice darker debris that isn’t pure wax and more of a wax-plus-skin
mix. The sensation is often itchier than painful, and it can flare with winter dryness or harsh cleansers. The best results usually come from reducing irritation (and resisting scratching),
not from aggressive wax removal.
The sudden “plugged ear” before a big event
A classic scenario: someone wakes up with one ear feeling blocked the day before travel, a wedding, or an important meetingbecause life has comedic timing.
Often the wax was already there, and a shower or sleep position shifts it just enough to seal the canal. The wax may look very dark when it finally comes out because it’s been sitting
for a while. In these cases, quick professional removal can be the fastest, safest way to restore hearing and comfort.
Final takeaway
Black earwax is often just older wax doing what wax doesdarkening with time and debris. But if it comes with pain, persistent itching, drainage, bleeding, or hearing changes, treat it as
a reason to get your ears checked rather than a sign to “clean harder.” The safest plan is usually the simplest: don’t dig, soften when appropriate, and let a clinician handle anything
that looks impacted or infected.