Table of Contents >> Show >> Hide
- First, a quick heart-terms translator
- Reality: What cardiac effects have been linked to COVID vaccination?
- Reality: How common is vaccine-associated myocarditisand how severe is it?
- Reality: COVID infection itself can hit the heart (and it’s not subtle)
- How we know: the U.S. safety systems that watch for heart-related signals
- The “Lies” section: Common mythsand what the evidence says instead
- Myth #1: “COVID vaccines cause widespread heart failure”
- Myth #2: “Any chest pain after a vaccine means your heart is inflamed”
- Myth #3: “Doctors are told to ignore myocarditis”
- Myth #4: “If there’s any myocarditis risk, vaccines must be ‘unsafe’”
- Myth #5: “They keep changing guidance because they’re lying”
- What symptoms should people take seriously?
- Risk reducers that show up in U.S. guidance
- How to fact-check scary heart claims in 60 seconds
- FAQ: Quick answers people actually want
- Conclusion: Reality is nuanced. Lies are loud.
- Experiences related to “COVID Vaccines and Cardiac Effects – Reality vs Lies” ()
If you’ve spent more than 30 seconds on the internet, you’ve probably seen it: a breathless post claiming COVID vaccines are
“destroying hearts,” “causing sudden death,” or “giving everyone myocarditis.” The comments section then turns into a digital
food fighthalf panic, half dunking, zero chill.
Let’s do something radical: look at what reputable U.S. medical and public-health sources actually say, what the data really
shows, and how to spot the difference between a legitimate safety concern and a viral fairy tale in a trench coat.
This article focuses on the main heart-related questions people ask about COVID-19 vaccinesespecially myocarditis and
pericarditiswithout sugarcoating, without fear-mongering, and without pretending your uncle’s Facebook meme has the same
credibility as national safety-monitoring systems.
First, a quick heart-terms translator
Myocarditis
Myocarditis means inflammation of the heart muscle (the myocardium). Inflammation can irritate heart tissue and, in some cases,
affect how the heart pumps or beats. Symptoms can include chest pain, shortness of breath, or palpitations (feeling like your
heart is racing or fluttering).
Pericarditis
Pericarditis is inflammation of the lining around the heart (the pericardium). It can also cause chest pain and discomfort,
sometimes sharp and worse with certain positions or deep breaths.
Important nuance: “inflammation” is not automatically “permanent damage.” Inflammation is a body response that can resolveoften
with rest and appropriate care. But it is something clinicians take seriously, which is exactly why it’s monitored so closely.
Reality: What cardiac effects have been linked to COVID vaccination?
1) Myocarditis/pericarditis (rare, but real)
U.S. safety monitoring and multiple studies support a causal link between mRNA COVID-19 vaccines (Pfizer-BioNTech and
Moderna) and rare cases of myocarditis/pericarditis, most often in adolescent and young adult males, frequently after a
later dose in the series. Regulators have updated product labeling over time to reflect evolving evidence and to communicate risk
clearly.
The risk is not the same for everyone. Across U.S. guidance, the pattern that shows up again and again is:
highest observed risk in males roughly in the teens through early 20s, with most cases occurring within about a week
after vaccination.
2) Other “heart events” you see online are often not caused by the vaccine
Posts sometimes claim vaccines cause heart attacks or “sudden cardiac death” broadly. Here’s the reality check:
when millions of people get vaccinated, some people will have medical events afterward simply because heart disease
and arrhythmias already happen every day in the populationespecially in older adults and people with existing risk factors.
That’s why scientists don’t rely on “it happened after” stories alone. They compare rates in vaccinated vs unvaccinated groups,
evaluate timing patterns, review medical records, and look for biological plausibility. That’s how you separate coincidence from
causation.
Reality: How common is vaccine-associated myocarditisand how severe is it?
The most honest answer is: it depends on age, sex, vaccine type, and dose timingbut overall, it’s rare.
Large surveillance systems and real-world studies find that the highest rates are still concentrated in a narrow demographic
(young males), and even there, the event remains uncommon relative to the number of doses given.
Severity matters just as much as frequency. The clinical picture described across major U.S. medical organizations and studies is
that many reported post-vaccine myocarditis cases are mild and improve with care. Follow-up research has looked at
outcomes beyond the initial hospitalization, because “what happens later?” is the question everyone deserves answered.
Bottom line: myocarditis is not something to wave awaybut the “everyone’s heart is being fried” storyline is not supported by
evidence.
Reality: COVID infection itself can hit the heart (and it’s not subtle)
One of the most misleading tricks in vaccine misinformation is comparing “vaccine risk” to “nothing.” But the real comparison is:
risk from vaccination vs risk from getting COVID.
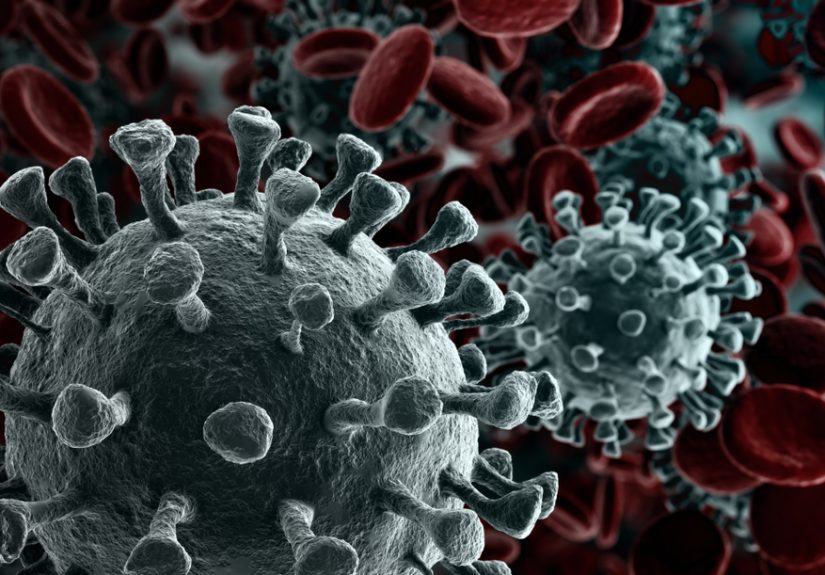
SARS-CoV-2 infection has been associated with myocarditis and other cardiac complications in multiple studies, including analyses
of large health-record datasets. In plain English: COVID can inflame the heart, stress the cardiovascular system, and trigger
complicationsespecially in people who get seriously ill, but not exclusively.
Many analyses conclude that the risk of myocarditis is generally higher after infection than after vaccination.
That doesn’t erase vaccine-associated myocarditis; it puts it in contextthe context that viral posts conveniently “forget.”
How we know: the U.S. safety systems that watch for heart-related signals
The U.S. doesn’t monitor vaccine safety by vibes. It uses overlapping systems designed to detect rare events:
-
VAERS (Vaccine Adverse Event Reporting System): An early-warning system. Anyone can report, so it’s great for
flagging patternsbut reports alone don’t prove causation. -
Active surveillance networks (e.g., large healthcare-database monitoring): These can compare vaccinated and
unvaccinated groups and evaluate risk by age/sex/dose. -
Clinical and epidemiologic investigations: Medical-record review, case definitions, expert panels, and follow-up
studies that look beyond the acute event.
This layered approach is one reason myocarditis/pericarditis was identified, characterized, and communicatedrather than hidden.
If your conspiracy theory requires thousands of hospitals, researchers, regulators, and clinicians to keep a perfect secret while
publishing peer-reviewed studies… your conspiracy theory needs better writers.
The “Lies” section: Common mythsand what the evidence says instead
Myth #1: “COVID vaccines cause widespread heart failure”
Reality: The primary heart-related safety signal consistently discussed is myocarditis/pericarditisrare, concentrated
in certain demographics, and often improving with care. Large studies and ongoing monitoring have not supported the claim of
widespread vaccine-caused heart failure across the general population.
Myth #2: “Any chest pain after a vaccine means your heart is inflamed”
Reality: Chest discomfort can come from many causesmuscle strain, anxiety/panic, reflux, respiratory infections,
and more. Clinicians evaluate symptoms carefully because chest pain deserves attention, but most post-vaccine chest pain is
not myocarditis.
Myth #3: “Doctors are told to ignore myocarditis”
Reality: U.S. clinical guidance explicitly tells clinicians to consider myocarditis/pericarditisespecially in
adolescents and young adults with certain symptomsevaluate appropriately, and report cases to safety systems. That is the
opposite of ignoring it.
Myth #4: “If there’s any myocarditis risk, vaccines must be ‘unsafe’”
Reality: In medicine, “safe” does not mean “zero risk.” It means the benefits outweigh the risks for the intended
population, with transparent communication and continuous monitoring. Even common medications have rare serious side effects; we
don’t pretend otherwisewe measure, manage, and communicate them.
Myth #5: “They keep changing guidance because they’re lying”
Reality: Guidance changes because evidence accumulates. Updating labels, intervals, and recommendations can reflect
better risk estimates, variant changes, and evolving benefit-risk profiles by age and health status. In science, changing your
mind when new data arrives is not a scandalit’s the job.
What symptoms should people take seriously?
If you or someone you care for develops acute chest pain, shortness of breath, or palpitationsespecially in the days
after vaccinationseek medical care promptly. This is not because “the vaccine is secretly dangerous.” It’s because these symptoms
can signal myocarditis, pericarditis, or other conditions that deserve evaluation.
If a clinician suspects myocarditis/pericarditis, they may use tools like an ECG and blood tests and decide whether imaging or
specialist follow-up is needed. If you’ve had myocarditis before, ask your clinician how that affects future vaccination decisions,
exercise timing, and monitoring.
(No, Googling your symptoms at 2 a.m. does not count as a cardiology fellowship. Sorry.)
Risk reducers that show up in U.S. guidance
Risk isn’t only about “shot or no shot.” Timing and product choices can matter. For example, U.S. public-health communications have
discussed that longer intervals between doses may be associated with lower myocarditis rates in some groups.
This kind of adjustment is a classic safety move: maintain protection while dialing down risk where possible.
Also, myocarditis/pericarditis concerns aren’t exclusive to mRNA products; U.S. safety pages note that data suggest an increased risk
following Novavax vaccination as wellanother example of monitoring that follows evidence, not brand loyalty.
Practical takeaway: the “safest” choice is individualized. Age, sex, health conditions, and local guidance all factor in.
A good clinician doesn’t dismiss concerns; they help you weigh them.
How to fact-check scary heart claims in 60 seconds
Step 1: Ask “What outcome, exactly?”
“Heart issues” is a fog machine of a phrase. Myocarditis? Pericarditis? Heart attack? Arrhythmia? “Sudden death” with no medical
details? Vague claims are harder to disprove and easier to share.
Step 2: Ask “Compared to what?”
If a post doesn’t compare vaccine risk to infection risk, it’s not analysisit’s marketing (and you’re the product).
Step 3: Check whether the source uses real surveillance language
Credible sources talk about case definitions, observed rates, age/sex patterns, uncertainty, and follow-up. Misinformation talks
about “they don’t want you to know,” sprinkled with screenshots and rage.
Step 4: Beware base-rate blindness
If 50 million people do something, you will see thousands of unrelated medical events afterwardbecause life keeps happening.
That’s why population studies exist.
FAQ: Quick answers people actually want
Is myocarditis after vaccination “new”?
Myocarditis itself isn’t new. It can happen after viral infections and, rarely, after other vaccines. What’s new is the scale of
monitoring and the sheer number of COVID-19 doses administered, which makes detection of rare patterns more likely.
Does vaccine myocarditis always cause lasting heart damage?
Not always. Many reported cases improve, and follow-up studies continue to examine outcomes over time. But any myocarditis diagnosis
warrants proper medical follow-up.
Should athletes worry?
Anyone diagnosed with myocarditiswhatever the causeshould follow clinician guidance on returning to exercise. That’s standard
cardiology practice, not a COVID-specific plot twist.
Does “rare” mean “ignore it”?
No. Rare means uncommon at the population level, not nonexistent. Good public health can say, “This is rare, here’s who’s most at
risk, here’s what to watch for, and here’s why benefits still matter.”
Conclusion: Reality is nuanced. Lies are loud.
The reality is refreshingly non-dramatic (which is probably why it doesn’t trend as hard):
COVID vaccines have a rare myocarditis/pericarditis risk, most notably in younger males, and U.S. agencies and medical
organizations have documented, monitored, and updated guidance and labeling accordingly.
The lies are dramatic (and algorithm-friendly): that hearts are being “ruined” at massive scale, that doctors are hiding evidence,
or that every chest twinge is proof of a cover-up. Those claims don’t hold up under surveillance data, clinical guidance, or
peer-reviewed research.
If you want to protect your heart, the best strategy isn’t to share the scariest headline. It’s to rely on evidence-based sources,
understand your personal risk factors, and talk to qualified healthcare professionals when symptoms or decisions feel uncertain.
Your heart deserves better than comment-section cardiology.
Experiences related to “COVID Vaccines and Cardiac Effects – Reality vs Lies” ()
Because this topic is so emotionally charged, people’s experiences often fall into a few recognizable bucketsand understanding
them helps separate reality from viral storytelling.
Experience pattern #1: “I felt chest pain, and I panicked”
A common story goes like this: someone gets vaccinated, and a day or two later they notice a weird chest sensationtightness,
soreness, or a sharp pain that comes and goes. They Google it. Google responds with the energy of a horror-movie narrator:
“It could be myocarditis.” Suddenly, every heartbeat becomes a plot point.
In real clinical settings, many of these cases turn out to be non-cardiacmuscle strain (yes, including from tense posture and
stress), reflux, or anxiety amplifying normal sensations. The key experience here isn’t “the vaccine harmed my heart.” It’s that
uncertainty plus online misinformation can turn ordinary symptoms into a full-blown spiral. The helpful move is the boring one:
get evaluated when symptoms are concerning, and let evidencenot fearrun the show.
Experience pattern #2: “It was myocarditisand it was treated seriously”
Another pattern is more straightforward: a teen or young adult (often male) develops noticeable chest pain and/or palpitations
within about a week of vaccination. They go in, clinicians check heart markers and an ECG, and myocarditis/pericarditis is
considered. The experience tends to be intense but structured: monitoring, guidance, and follow-up. People often describe
relief that it was recognized quicklybecause they’d been told “no one talks about it,” then discovered clinicians talk about it
constantly, precisely because it’s a known (rare) possibility.
Many individuals describe gradual improvement over days to weeks, with medical guidance around rest and returning to activity.
The emotional whiplash is real: “I was scared because the internet said my heart was permanently damaged,” followed by “my
cardiology follow-up was calm, specific, and focused on recovery.”
Experience pattern #3: “People use my story as propaganda”
Some people who’ve had myocarditiswhether related to vaccination, infection, or another causereport a frustrating side effect:
strangers try to recruit them into a narrative. If they mention vaccine timing, they get pushed to say “vaccines are poison.”
If they emphasize recovery and context, they get accused of being “paid” or “brainwashed.” In other words, their real medical
experience gets flattened into a social-media talking point.
Experience pattern #4: “COVID itself messed with me more than the shot”
Plenty of people describe lingering symptoms after infectionfatigue, racing heart, chest discomfort, exercise intolerance
sometimes under the umbrella of post-COVID conditions. These experiences don’t always get the same viral attention as “vaccine
injury” posts, but they’re part of the real-world landscape clinicians see. It’s a reminder that the risk conversation is not
“vaccine vs perfect health.” It’s “vaccine vs a virus that can also stress the cardiovascular system.”
Taken together, these experiences point to the same conclusion: reality is complicated and individualized, while lies are
one-size-fits-all. If you’re making health decisions, you deserve better than a memeyou deserve context, data, and professional
guidance.