Table of Contents >> Show >> Hide
- Why these two symptoms often travel together
- Common (and usually short-term) causes
- Medical causes that deserve a closer look
- When to see a doctor (and when to seek urgent care)
- What a clinician may ask (and what tests might be ordered)
- What you can do right now (safe, practical steps)
- FAQ
- Real-life experiences with fatigue and loss of appetite (the “this is what it actually feels like” section)
Fatigue + loss of appetite is one of those annoying “two-for-one” symptom combos: you’re running on low battery and food suddenly feels as appealing as doing taxes on a roller coaster. The tricky part is that these symptoms are common and nonspecific. They can show up with everyday issues (poor sleep, a virus, dehydration), but they can also be early signals of something that deserves medical attention.
This guide breaks down the most likely causes, the red flags that should move you from “I’ll nap it off” to “I should call my doctor,” and practical ways to cope while you figure out what’s going on.
Why these two symptoms often travel together
Energy and appetite are tightly connected. When your body is under stresslike fighting an infection, running low on fluids, dealing with inflammation, or navigating mental health strainit may conserve resources. That can look like:
- Lower energy (fatigue, weakness, brain fog)
- Lower hunger signals (reduced appetite, early fullness, “meh” toward food)
Sometimes appetite drops first, then fatigue follows because you’re not fueling well. Other times fatigue hits first, and appetite fades because you’re too wiped out to cook, chew, or care.
Common (and usually short-term) causes
1) Viral illnesses and “sick season” stuff
Respiratory viruses (like flu and COVID-19) commonly cause fatigue, and many people also experience nausea, stomach upset, or just a general “no thanks” to food. Even a typical cold can leave you tired, especially if it disrupts sleep.
Clues it’s a short-term bug: symptoms began suddenly, you’ve got body aches or fever, you feel worse for a few days, then slowly improve.
2) Dehydration (even mild dehydration)
Dehydration can make you feel tired, lightheaded, and surprisingly uninterested in eating. If you’re sick, sweating, not drinking much, or losing fluids through vomiting/diarrhea, dehydration can become a major driver of both symptoms.
Helpful signs to check: darker urine, dry mouth, headache, dizziness, rapid heart rate, or feeling “off” when standing up.
3) Not eating enough (or not eating well)
Skipping meals can lead to fatigueand fatigue can make meal prep feel like climbing Everest in flip-flops. This creates a loop: less food → less energy → less appetite → less food.
If you’ve been stressed, busy, nauseated, or relying on low-nutrient snacks, your body may be asking for a reset.
4) Poor sleep, stress, burnout, and overtraining
Chronic stress and sleep debt can blunt hunger cues and raise fatigue. Overtraining can also do it: your body may feel depleted, inflamed, and strangely uninterested in foodeven though you actually need more fuel.
Clue: symptoms build gradually, and you notice mood changes, irritability, or reduced performance at work or workouts.
5) Medication side effects (and alcohol/substances)
Many medications can affect appetite or energy. Some cause nausea, taste changes, or sleep disruption. Alcohol and recreational substances can also interfere with sleep quality, stomach comfort, hydration, and overall energymaking fatigue and appetite loss more likely.
Clue: symptoms started after a new medicine, a dose change, or increased alcohol use.
Medical causes that deserve a closer look
If fatigue and loss of appetite are persistent (for example, more than a week or two without clear improvement), recurrent, or paired with concerning symptoms, it’s worth considering medical causes. Here are some of the more common “bigger picture” categories clinicians think about.
Anemia
Anemia can reduce oxygen delivery to tissues, which often shows up as fatigue, weakness, shortness of breath with exertion, dizziness, or headaches. The underlying cause matters (iron deficiency, vitamin deficiencies, chronic disease, blood loss), and treatment depends on the type.
Clues: unusual tiredness, paleness, rapid heartbeat, shortness of breath, dizzinessespecially if symptoms are new or worsening.
Thyroid problems (especially hypothyroidism)
An underactive thyroid can slow body processes and contribute to fatigue, low mood, constipation, feeling cold, and changes in weight. Symptoms can be subtle and overlap with many other conditionsblood tests help clarify.
Clues: fatigue that doesn’t match your lifestyle, feeling cold, dry skin, constipation, low mood, “brain fog.”
Depression (and other mental health conditions)
Depression isn’t only sadnessit can show up as low energy, poor concentration, sleep disruption, and appetite changes (often reduced appetite, sometimes increased). When fatigue and appetite loss come with loss of interest, hopelessness, or persistent low mood, mental health deserves equal attention as physical health.
Clues: symptoms persist most days for 2+ weeks, plus low mood, loss of pleasure, sleep changes, guilt, or difficulty functioning.
Kidney disease
Chronic kidney disease can cause vague symptoms that creep in over timefatigue, nausea, appetite loss, itching, and changes in urination. Many people have few symptoms until later stages, so evaluation is important if symptoms persist or you have risk factors (high blood pressure, diabetes, family history).
Clues: persistent nausea, itching, swelling, changes in urination, fatigue that keeps worsening.
Liver disease (including cirrhosis)
Liver problems can cause fatigue, poor appetite, nausea, weight loss, and itching. Symptoms may be mild at first and become more noticeable as disease progresses. Risk factors include heavy alcohol use, viral hepatitis, and metabolic conditions linked to fatty liver disease.
Clues: persistent fatigue plus nausea, itching, abdominal discomfort, yellowing of skin/eyes, easy bruising, or swelling.
Heart failure and other heart conditions
Heart failure can reduce the body’s ability to meet oxygen and nutrient demands, contributing to fatigue. Some people also experience reduced appetite or nausea. Because heart symptoms can be easy to misread as “just getting older,” persistent changes deserve attention.
Clues: shortness of breath (especially with activity or when lying flat), swelling in legs/ankles, rapid weight gain from fluid, fatigue that limits daily activity, appetite changes.
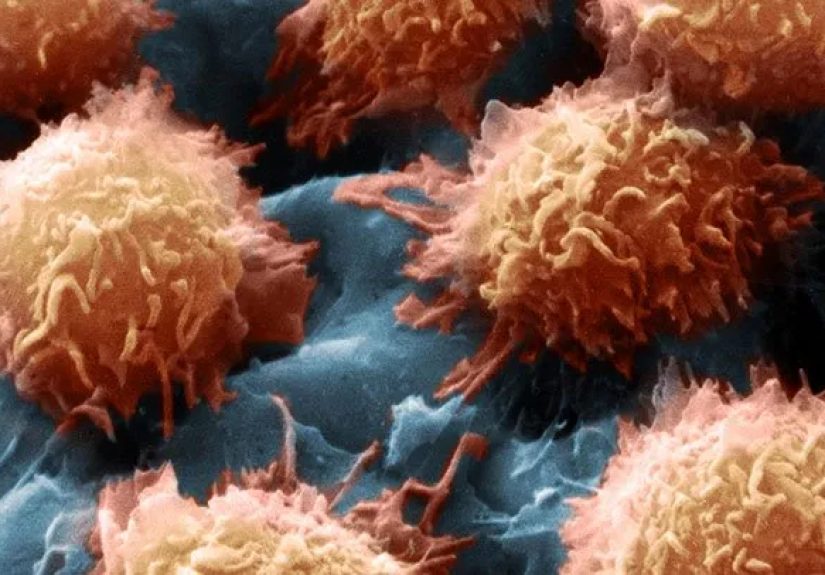
Cancer and cancer treatment effects
It’s important not to jump to worst-case conclusionsmost people with fatigue and appetite loss do not have cancer. But persistent, unexplained fatigue and appetite loss can sometimes be associated with cancer or its treatments, especially when paired with unintentional weight loss, ongoing pain, fevers, night sweats, or bleeding.
Clues: symptoms persist and progress, plus unintentional weight loss, new lumps, persistent fevers, night sweats, or ongoing gastrointestinal symptoms.
Addison’s disease (less common, but important)
Addison’s disease (adrenal insufficiency) can include long-lasting fatigue, muscle weakness, loss of appetite, weight loss, and lightheadedness. It’s uncommon, but clinicians consider it when symptoms cluster in a suggestive way or don’t fit more common explanations.
When to see a doctor (and when to seek urgent care)
If you’re unsure, it’s always reasonable to check in with a clinicianespecially if symptoms are interfering with daily life. Consider getting prompt medical advice if you have:
- Fatigue and poor appetite lasting more than 1–2 weeks, or worsening over time
- Unintentional weight loss
- Fainting, confusion, or severe weakness
- Shortness of breath, chest pain, or new swelling
- Persistent vomiting, inability to keep fluids down, or signs of dehydration
- High fever that persists or returns
- Blood in stool or vomit, black/tarry stools, or severe abdominal pain
- Yellowing of the skin/eyes or dark urine with pale stools
- New severe depression or thoughts of self-harm (seek immediate help)
What a clinician may ask (and what tests might be ordered)
Because these symptoms can come from many directions, clinicians usually start with detective work:
Questions you’ll likely get
- When did it start? Sudden vs gradual?
- Any recent infection exposure, travel, or major stress?
- Any weight change, fever, night sweats, pain, bowel changes?
- Sleep quality, mood, anxiety, workload, training changes?
- Medications, supplements, alcohol, or substance use?
- Diet pattern and hydration (especially if nausea is involved)
Common tests (depending on your situation)
- Blood counts (to evaluate anemia and infection)
- Metabolic panel (electrolytes, kidney and liver markers)
- Thyroid testing
- Inflammation markers or specific tests if infection is suspected
- Urinalysis for hydration and kidney clues
- Other tests or imaging if red flags or persistent symptoms suggest a specific direction
Translation: the goal isn’t to run every test ever invented. It’s to pick smart tests based on your pattern of symptoms.
What you can do right now (safe, practical steps)
While you’re monitoring symptoms or waiting for an appointment, these strategies are generally helpful and low-risk.
1) Hydrate like it’s your side quest
Small sips throughout the day can be easier than chugging. If you’ve had vomiting/diarrhea or heavy sweating, an oral rehydration solution or electrolyte drink can help replace salts as well as fluids.
2) Eat “low-effort, high-return” foods
When appetite is low, aim for small, frequent, nutrient-dense options:
- Soups or broths (bonus hydration)
- Smoothies with yogurt or nut butter
- Eggs, oatmeal, toast, rice, bananas
- Trail mix, cheese, crackers, hummus
If nausea is part of the story, bland foods and smaller portions often feel better than greasy or heavily spiced meals.
3) Protect your sleep (even if you can’t “sleep it off”)
Consistent wake time, reduced late caffeine, and a calmer bedtime routine can help. Poor sleep doesn’t just cause fatigueit can also disrupt appetite regulation.
4) Do a gentle symptom diary for 3–7 days
Track: energy level, appetite, weight (optional), fever, hydration, bowel changes, new meds, stress, and sleep. Patterns help cliniciansand help you notice what improves or worsens symptoms.
5) Be cautious with “energy hacks”
Extra caffeine can reduce appetite and worsen sleep. If you’re already drained, adding jittery energy isn’t always a win. Think “steady” over “spiky.”
FAQ
How long is “normal” for fatigue and appetite loss?
If it’s tied to a short-term illness, many people start improving within several days. If you’re not seeing any improvement after 1–2 weeks, or symptoms are worsening, that’s a good time to check in with a healthcare professional.
Can stress really do this?
Yes. Stress can disrupt sleep, digestion, and hunger cues. But stress can also mask other conditions. If symptoms are persistent, don’t assume it’s “just stress” without a check-in.
What if I’m hungry sometimes but still exhausted?
That can still happen with anemia, sleep disorders, depression, thyroid issues, infections, or chronic medical problems. Appetite is only one clueyour overall symptom pattern matters more.
Real-life experiences with fatigue and loss of appetite (the “this is what it actually feels like” section)
Experience #1: The “I thought it was just a cold” week.
A lot of people describe a viral illness as a sudden energy crash: one day you’re fine, the next you’re moving like your limbs are made of wet laundry. Appetite often drops because your senses feel dull, swallowing feels annoying, or your stomach is unsettled. The turning point usually comes when hydration improves and sleep finally catches upoften after a few days of simple meals, naps, and accepting that being productive is temporarily canceled.
Experience #2: The dehydration spiral.
Some folks don’t realize dehydration is the main problem until they notice the little tellsdry mouth, headache, dizziness, darker urine, and a weird lack of hunger. They might keep skipping meals because “nothing sounds good,” but once they start sipping fluids regularly (and adding electrolytes when needed), appetite often begins to return. The biggest lesson people report: hydration isn’t only about thirst; it’s also about energy and appetite.
Experience #3: Burnout wears a lab coat sometimes.
People dealing with prolonged stress often describe fatigue as “wired but tired”exhausted, but restless. Appetite can become inconsistent: forgetting to eat, eating only snacks, or feeling full too quickly. What surprises many is that the body can feel physically ill from mental overload. When they finally rebuild a routineconsistent wake time, actual meals, and boundaries around workboth energy and appetite often improve. And when they don’t, that’s frequently what pushes them to get checked for anemia, thyroid issues, or depression.
Experience #4: The “it wasn’t just aging” realization.
Some people (or their family members) chalk up persistent fatigue to getting olderuntil stairs feel harder, daily chores take longer, and appetite fades. That’s when symptoms like swelling, shortness of breath, or ongoing nausea become impossible to ignore. Many describe relief after evaluationnot because the diagnosis is fun, but because there’s a reason and a plan. The big takeaway is that persistent fatigue and appetite loss aren’t “normal,” at any age, if they’re changing your baseline.
Experience #5: The slow-burn deficiency story.
A common pattern with anemia or nutrient deficiencies is gradual decline: you don’t wake up one day dramatically illyou just become less you over time. People report needing more naps, feeling winded sooner, and losing interest in food because they feel vaguely unwell. The “aha” moment often happens after routine bloodwork. The experience can be frustrating (“Why didn’t I notice sooner?”) but also empowering: many cases improve when the underlying cause is identified and treated.
Final takeaway: Fatigue and loss of appetite are signals, not diagnoses. If they’re brief and clearly tied to a minor illness or a chaotic week, supportive care may be enough. If they’re persistent, worsening, or paired with red flags, getting evaluated is a smart movenot a dramatic one. Your body isn’t being mysterious to annoy you. It’s sending a message. The goal is to decode it.