Table of Contents >> Show >> Hide
- Quick refresher: What is type 2 diabetes, and why does risk climb?
- What “Mediterranean diet” actually means (and what it doesn’t)
- The evidence: Why experts keep pointing to Mediterranean-style eating
- So why does it work? The “how” behind the hype
- “More effective” than what, exactly?
- How to do the Mediterranean diet for diabetes risk reduction (U.S.-friendly)
- What about carbscan you still eat pasta?
- Don’t forget the lifestyle piece: food + movement is the power combo
- Common mistakes (and how to dodge them like a pro)
- Who benefits mostand who should personalize it?
- Bottom line: Mediterranean-style eating is a smart, realistic strategy
- Experiences: What It’s Like to Actually Live the Mediterranean Diet (In Real Life)
- The first surprise: You’re fuller than expected
- Grocery shopping feels different (but in a good way)
- The “I miss fast food” phaseand how people get past it
- Restaurant life doesn’t endpeople just order smarter
- People often notice better energy (and fewer “afternoon crashes”)
- The long-term experience: It becomes “how I eat,” not “a plan I’m on”
If type 2 diabetes had a “most annoying” award, it would win every year. It sneaks up quietly, hangs around forever,
and makes you read nutrition labels like you’re studying for the bar exam. The good news: type 2 diabetes is often
preventable (or at least delayable), and one of the strongest dietary patterns linked to lower risk is the
Mediterranean dietespecially when it replaces the ultra-processed, drive-thru-heavy “modern Western” style of eating.
But is the Mediterranean diet really more effective? In a nutshell: it’s one of the most evidence-backed,
most sustainable eating patterns for reducing type 2 diabetes risk, and in some large studies it has beaten a standard
low-fat control approachsometimes by a lot. Even better, it doesn’t require you to swear off carbs forever or live on
chicken breast and sadness.
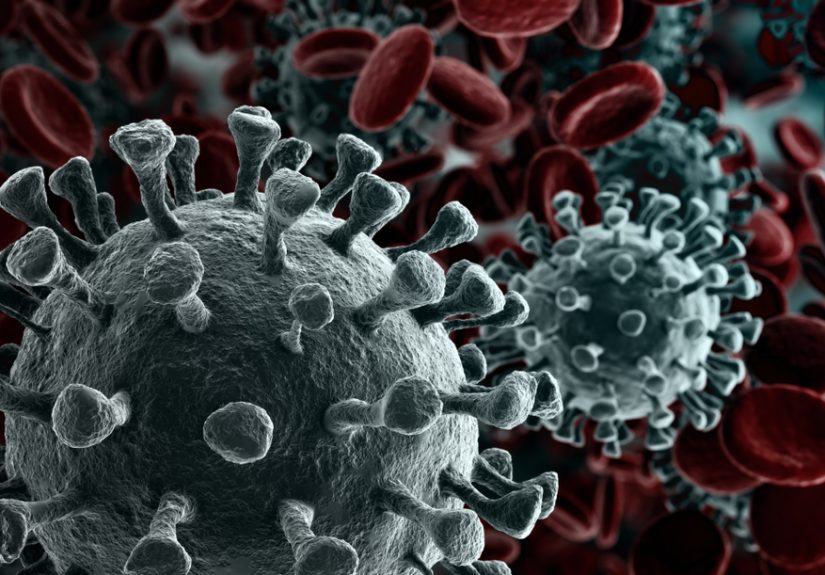
Quick refresher: What is type 2 diabetes, and why does risk climb?
Type 2 diabetes happens when your body becomes resistant to insulin (the hormone that helps move glucose from your
bloodstream into your cells), and/or your pancreas can’t keep up with insulin demand. Over time, blood glucose stays
elevated, which can damage blood vessels and nervesraising the risk of heart disease, kidney disease, vision problems,
and more.
Risk isn’t random. Common factors include having prediabetes, carrying extra weight (especially around the abdomen),
being less physically active, family history, age, a history of gestational diabetes, and certain health conditions.
Your risk can also vary across populations due to a mix of genetics, access to care, environment, and social factors.
Translation: this is not a “willpower” issueit’s a biology-plus-life-circumstances issue.
What “Mediterranean diet” actually means (and what it doesn’t)
The Mediterranean diet isn’t a strict meal plan. It’s a patterncommon in traditional cuisines around the Mediterranean
Seathat emphasizes:
- Vegetables, fruits, beans, lentils, and whole grains (fiber is the unsung hero here)
- Healthy fatsespecially extra-virgin olive oil (a.k.a. “liquid gold”)
- Nuts and seeds (small but mighty)
- Fish and seafood more often; poultry and eggs in moderation
- Less red and processed meat
- Fewer sweets and ultra-processed foods
- Optional alcohol, typically wine with meals (not a requirement and not recommended to start if you don’t drink)
What it does not mean: drowning everything in olive oil and calling it health. Olive oil is great, but it’s
still calorie-denseyour salad shouldn’t need a lifeguard.
The evidence: Why experts keep pointing to Mediterranean-style eating
1) It has strong research behind itincluding randomized trials
Many diets have fans. The Mediterranean diet has receipts.
In a major randomized trial (often discussed in diabetes research), people at high cardiovascular risk who followed a
Mediterranean-style diet supplemented with either extra-virgin olive oil or mixed nuts experienced a substantially lower
incidence of new type 2 diabetes compared with a low-fat control approach. Notably, the reduction in diabetes risk
showed up even without big differences in weight changesuggesting benefits beyond “just lose weight.”
More recent research also suggests that when a Mediterranean-style pattern is combined with lifestyle supportslike
modest calorie reduction, regular physical activity, and structured coachingdiabetes risk can drop meaningfully over
years. That combination matters because real-world prevention isn’t one magic ingredient; it’s a set of doable habits
that stack.
2) Major health organizations include it among evidence-based patterns
The Mediterranean pattern is frequently listed among eating approaches supported by evidence for preventing or managing
diabetes. It’s also widely recommended for cardiovascular healthwhich matters because type 2 diabetes and heart disease
are close friends, and not the fun kind.
So why does it work? The “how” behind the hype
Fiber slows the glucose roller coaster
Mediterranean-style meals are naturally high in fiber from vegetables, legumes, whole grains, nuts, and seeds. Fiber
slows digestion and reduces sharp blood sugar spikes after meals. It also helps with fullness, which can support weight
management without feeling like you’re rationing joy.
Healthy fats improve the overall metabolic environment
Replacing saturated fats (common in fatty meats, butter, some ultra-processed foods) with unsaturated fats (olive oil,
nuts, seeds, fish) is associated with better cardiometabolic health. For diabetes prevention, this matters because
insulin resistance and inflammation often travel together like an annoying duo in a buddy comedy.
It pushes out ultra-processed foods without a “ban list” vibe
A big reason the Mediterranean pattern is effective is what it displaces: sugar-sweetened beverages, refined grains,
packaged snacks, and other ultra-processed foods that tend to be high in calories and low in fiber and micronutrients.
You’re not “on a diet.” You’re just eating more real foodso there’s less room for the stuff that doesn’t help.
It’s sustainableand sustainability is a secret weapon
The best diet for diabetes risk reduction is the one you can still do when life gets messywhen work is busy, the kids
are hungry, or you’re traveling. Mediterranean-style eating works well in the U.S. because it’s flexible: you can do it
at the grocery store, at restaurants, and even (with a little strategy) at barbecues.
“More effective” than what, exactly?
Here’s the honest, grown-up answer: Mediterranean-style eating is often more effective than a typical Western pattern
and has outperformed a standard low-fat control in some research settings. But it isn’t the only evidence-based option.
Other high-quality patternslike DASH, lower-carbohydrate approaches for some people, and plant-forward dietary patterns
may also reduce risk or improve blood sugar markers.
Think of it like exercise: walking, cycling, and swimming can all improve fitness. Mediterranean is the “walking” of
diets (‘simple, effective, doesn’t require special equipment’), and for a lot of people it’s the easiest to keep doing.
How to do the Mediterranean diet for diabetes risk reduction (U.S.-friendly)
Use the “Mediterranean Plate” (no calculator required)
- Half the plate: non-starchy vegetables (salad, broccoli, peppers, green beans, cauliflower, etc.)
- Quarter of the plate: protein (fish, beans, lentils, chicken, tofu, Greek yogurt)
- Quarter of the plate: high-fiber carbs (brown rice, quinoa, oats, farro, whole-grain pasta, sweet potato)
- Add: olive oil + nuts/seeds in sensible amounts
Swap this → for that (small changes that add up)
- Butter or creamy sauces → olive oil + lemon + herbs
- Chips or cookies daily → nuts + fruit (still satisfying, less blood sugar drama)
- White bread → whole-grain bread (check for whole grains listed first)
- Processed deli meats → tuna, salmon, beans, rotisserie chicken
- Sugary drinks → water, sparkling water, unsweetened tea
A simple 1-day Mediterranean-style menu (with realistic portions)
Breakfast: Greek yogurt with berries + chopped walnuts + cinnamon. Optional: a slice of whole-grain toast with olive oil drizzle or avocado.
Lunch: Big salad (greens, tomatoes, cucumbers, chickpeas) + grilled chicken or canned salmon + olive oil & vinegar dressing + whole-grain pita.
Snack: Apple + peanut butter, or hummus + carrots.
Dinner: Baked salmon with lemon and herbs + roasted vegetables + quinoa or farro. Optional: fruit for dessert.
What about carbscan you still eat pasta?
Yes, you can still eat pasta. The Mediterranean pattern doesn’t demonize carbs; it upgrades them. The goal is to choose
higher-fiber carbs more often and keep portions reasonableespecially if you have prediabetes or a history of elevated
blood sugar.
Three practical rules:
- Choose whole grains when you can (whole-grain pasta, oats, brown rice).
- Pair carbs with protein and fat (pasta + beans + olive oil + veggies beats pasta alone).
- Let vegetables be the volume so the meal is filling without being carb-heavy.
Don’t forget the lifestyle piece: food + movement is the power combo
Diet matters, but diabetes prevention research consistently shows that lifestyle changes work best as a bundle. Large
studies have found that modest weight loss and regular physical activity can significantly cut the progression from
prediabetes to type 2 diabetes. The Mediterranean pattern fits beautifully here because it supports fullness, nutrient
density, and heart healthso it’s easier to sustain alongside movement goals.
If you want an easy starting target: aim for regular movement you can repeat (like brisk walking) and build up gradually.
Your body doesn’t need perfection. It needs consistency.
Common mistakes (and how to dodge them like a pro)
Mistake #1: “Mediterranean” becomes “I added olive oil to pizza”
Olive oil is excellent, but it’s not a magical shield. Keep the foundation plant-forward: vegetables, beans, whole
grains, fish, nuts. Then add olive oil as the main fat.
Mistake #2: Going “healthy” but not getting enough protein
Protein supports satiety and steadier blood sugar. If lunch is just salad and vibes, you may end up raiding the pantry
at 4 p.m. Add chickpeas, tuna, chicken, tofu, or Greek yogurt.
Mistake #3: Treating wine as a requirement
Mediterranean-style eating sometimes includes moderate wine, but it’s optionaland not recommended for everyone.
If you don’t drink, don’t start for “health.” You can get the benefits without alcohol.
Mistake #4: Forgetting sodium and added sugars
Mediterranean doesn’t automatically mean low-sodium or low-sugarespecially if you rely on packaged “Mediterranean”
snacks or restaurant meals. Read labels for added sugars and use herbs, lemon, garlic, and spices to boost flavor
without turning your blood pressure into a trampoline.
Who benefits mostand who should personalize it?
Mediterranean-style eating is generally safe and beneficial for most adults, including those with prediabetes and many
people with type 2 diabetes. But personalization matters if you:
- Have kidney disease (protein/potassium/phosphorus may need adjustment)
- Use glucose-lowering medications (meal timing and carb distribution matter)
- Have celiac disease (choose gluten-free whole grains like quinoa, brown rice, certified GF oats)
- Have food allergies (nuts, fisheasy swaps exist)
If you’re managing blood sugar concerns, consider meeting with a registered dietitianespecially one who understands
diabetes care. A little personalization can turn “good” into “works perfectly for me.”
Bottom line: Mediterranean-style eating is a smart, realistic strategy
The Mediterranean diet earns its reputation because it’s not a gimmickit’s a practical pattern supported by strong
research, and it aligns with what we know about preventing type 2 diabetes: more fiber, more whole foods, better fats,
fewer ultra-processed items, and a lifestyle you can actually live with.
If you want to start today, don’t overhaul your entire kitchen at once. Pick one change:
swap butter for olive oil, add beans twice this week, or aim for vegetables at two meals a day. The “Mediterranean”
part isn’t a passport stampit’s a set of habits. And those habits can add up to a meaningful reduction in diabetes risk.
Experiences: What It’s Like to Actually Live the Mediterranean Diet (In Real Life)
Let’s talk about the part that research papers rarely capture: the human experience. Not “a participant
demonstrated statistically significant improvement,” but “what do people notice when they try this at homebetween work
meetings, grocery budgets, and a family member who thinks vegetables are decorative?”
The first surprise: You’re fuller than expected
Many people expect a “healthy diet” to mean constant hunger. Mediterranean-style eating often flips that script because
it’s naturally high in fiber (vegetables, beans, whole grains) and includes satisfying fats (olive oil, nuts). A common
experience is realizing: “Wait… I ate a big bowl of lentil soup with a salad and I’m not hunting for snacks an hour later.”
That satiety can make it easier to reduce mindless grazingone of the quiet drivers of unwanted weight gain and blood
sugar instability.
Grocery shopping feels different (but in a good way)
People often describe a “perimeter-first” shift: more time in produce, seafood, dairy, and bulk grains; less time in the
snack aisle where everything is neon, crunchy, and suspiciously dusted with “nacho flavor.” A practical hack many adopt
is building a repeatable cart:
- 2–3 vegetables they’ll actually eat (bagged salad counts; we’re not here to judge)
- 1–2 fruits for snacks
- 1–2 proteins (canned tuna/salmon, chicken, eggs, tofu)
- 1 bean/legume option (chickpeas, lentils, black beans)
- 1 whole grain (oats, brown rice, quinoa, whole-grain pasta)
- Olive oil, nuts, and a couple of “make it taste good” items (garlic, lemons, salsa, herbs, spices)
The “I miss fast food” phaseand how people get past it
A common bump is the first 1–2 weeks when cravings for ultra-processed foods show up like uninvited guests. People
report that having “Mediterranean convenience foods” on hand helps: hummus, rotisserie chicken, pre-cut veggies, frozen
fish fillets, microwavable brown rice, and canned beans. The experience becomes less about willpower and more about
making the healthy choice the easy choice.
Restaurant life doesn’t endpeople just order smarter
A surprisingly positive experience is realizing you can do Mediterranean-style eating at restaurants without sounding
like you’re auditioning for a nutrition documentary. Common wins:
- Choosing grilled fish or chicken and swapping fries for a side salad or vegetables
- Asking for dressing on the side and using olive oil + vinegar when available
- Leaning into cuisines that already fit the pattern (Greek, Middle Eastern, many Italian options, seafood spots)
- Splitting dessertsor choosing fruitbecause you actually feel satisfied after the meal
People often notice better energy (and fewer “afternoon crashes”)
While everyone’s body is different, many describe fewer energy slumps when lunches include protein, fiber, and healthy
fats instead of refined carbs alone. Think: salad + beans + chicken + olive oil dressing versus a giant white-bread
sandwich and chips. The second one tastes great… right up until it turns your afternoon into a nap negotiation.
The long-term experience: It becomes “how I eat,” not “a plan I’m on”
The biggest “experience advantage” people mention is that the Mediterranean pattern doesn’t feel like punishment.
There’s flavor. There’s flexibility. There’s room for cultural foods and family meals. Over time, many end up with a
default rotationsheet-pan salmon, bean chili, veggie omelets, Greek yogurt bowls, hearty salads, whole-grain pasta with
roasted vegetablesso the diet stops being a project and starts being a routine.
If you’re using this approach specifically to reduce type 2 diabetes risk, the lived experience tends to be best when
you keep the goal simple: more plants, better fats, steady protein, and fewer ultra-processed foodsmost days. Progress
doesn’t require perfection. It requires a pattern you can repeat.